Rama Ranee
|
February 23, 2026
|
12
min read
Raised by nature: Bonds with farms, forests help children grow holistically
Safe spaces, outlets for creativity and curiosity, and a connection to the Earth—nature can mean many things to kids
Read More

With a more diverse diet, this tight-knit community is able to achieve greater food security in harsh winters
If you were to arrive at Ladakh’s Kesar early in the evening, you’d find the whole village—all of 17 women and a handful of children—seated in a circle on the grey, sandy earth of someone’s backyard, using loose wooden floorboards as mats. You’ll see women in salwar suits and sweaters, wearing scarves over their heads and socks under their slippers. You’ll see a pink-and-white ceramic tray with matching pink-and-white ceramic cups, and a thermos or two of tea. The men of the village live wherever they find employment—mostly in Leh, where they work as drivers. The women stay back, raising children, growing crops, and keeping the village alive.
Kesar village is located on the Changthang Plateau, over 4,000 metres above sea level. It is dry, bitingly cold desert land, barren for most of the year. In the winter months, the mercury plummets to temperatures as low as -30°C. From May to September, there opens a small window of time when the women of the village can grow wheat, barley, and potatoes. This wheat, once it has been harvested and cleaned, is either ground into flour (atta) or dry roasted to make sattu. It serves as their primary food for the rest of the year, weaving itself into their sparse diet: rotis with dal for their main meals, and sattu with their tea. Little else adds colour or variety to their food. For vegetables, they were dependent on a weekly bus to Leh—the closest city, over 180 km away—but they could barely afford it.
The spaces between the layers of polycarbonate trap air, creating air pockets that keep warm air from escaping, maintaining warmth within the greenhouse even in sub-zero temperature winters.
In 2023, the Sher-e-Kashmir University of Agricultural Sciences and Technology (SKUAST, Jammu) introduced polyhouse farming to the region and trained the village women in controlled-environment agriculture. Polyhouses function as advanced greenhouses made of brick walls and plastic roofs; they trap solar radiation and maintain warmth to allow for year-round cultivation of vegetables. The polyhouse in Kesar village features three sides of mud brick walls for improved heat retention, and a triple-layer polycarbonate sheet, chosen for its durability compared to other types of plastics, as well as its ability to diffuse more light than glass. Moreover, to maximise the sunlight received, the polycarbonate sheet typically faces south. The spaces between the layers of polycarbonate trap air, creating air pockets that keep warm air from escaping, maintaining warmth within the greenhouse even in sub-zero temperature winters.
{{marquee}}
Polyhouses have been transformative for the village. While they continue to buy pulses from Leh, they now eat the vegetables they grow. Tsering Lamo, one of Kesar’s residents, talks about how the polyhouses have brought food security—something she didn’t have while growing up. “But now, everything is alright,” she says. “We have vegetables, grains—everything.” The polyhouse has also infused variety into their diet. Instead of living on just dal to accompany their rotis, they now have vegetables. This gives them a reason to cook twice a day, and to find creative ways to incorporate their produce into meals. These vegetables also add new twists to familiar dishes like momos.
The polyhouse has also infused variety into their diet. Instead of living on just dal to accompany their rotis, they now have vegetables.
For miles around, there are only two colours visible: brown and grey. The sky, the mountains, the land—even the sparse vegetation—conform to the palette. The landscape appears majestic and imposing, but also distant and spiritless. The air is suffused with loneliness. In response, a sisterhood has come alive—one that grows food together, cooks together, and eats together. At night, they break off into smaller groups, eating dinner and sleeping over at each other’s houses—living life in an ongoing, alternating sleepover. The polyhouse becomes another weapon in their arsenal; another way to stave off loneliness. Not only are they solving their food problem, but they are also having fun with it, bringing a sense of curiosity, experimentation, and purpose to their time in the polyhouse. They’ve grown not only common polyhouse crops like lettuce, cucumbers and potatoes, but also small watermelons. “This is a newly set-up greenhouse, and we’re slowly figuring out what else we can grow here,” says Tsering Zangmo, with a spark in her eyes.
If you pass them by, the sisterhood will cheerfully call out: “Juley! Juley! Juley!” Juley is used to convey many things—hello, welcome, please, and thank you—with the singular feeling of warmth. The sisterhood of the cold desert thrives.
Also read: Sasbani’s 'fruits' of labour: Reviving hope in rural Uttarakhand
Also read: At Ammachi’s farm, the impossible can be achieved—and made profitable
{{quiz}}

From nutrient imbalance to kidney stress, here’s what happens when your diet contains excess protein
Editor's Note: From grocery lists, to fitness priorities, and even healthy snacking, protein is everywhere—but do we truly understand it? In this series, the Good Food Movement breaks down the science behind this vital macronutrient and its value to the human body. It examines how we absorb protein from the food we consume, how this complex molecule has a role to play in processes like immunity, and the price the Earth pays for our growing protein needs.
Over the last decade, the global food industry has flooded the market with ‘proteinified’ products, heavily capitalising on the widespread belief that we are constantly falling short on the macronutrient. And it’s not just supplements, bars or shakes anymore, people. Those bowing to the fitness holy grail have the option to buy protein-packed ice cream, soda, pasta and even popcorn!
But this surge has less to do with our nutritional needs, and more with clever marketing. As the Wall Street Journal put it back in 2013: “When the box says ‘protein,’ shoppers say ‘I’ll take it’.” This constant messaging that we aren’t eating enough has created a certain ‘protein anxiety’.
Protein is essential for building and repairing tissues. However, consistently consuming it in excess can trigger health issues.
Protein needs do not remain constant over the human lifespan. For the average adult, 0.8-1 gram of protein per kilogram of body weight per day is sufficient. Getting more than 22% of daily calories from protein may do more harm than good. For most adults, about 20–30 grams of protein per meal—or 60–90 grams per day—is enough to stay healthy. Active individuals (especially those doing weight training for more than an hour daily) may need slightly more than this baseline threshold.
Other needs vary more dramatically. Pregnant and lactating women usually need more for bodily repair and growth. Those with chronic illness or inflammation also have greater needs since their bodies use and break down protein faster. Older adults often require more to maintain muscle mass. Ironically, the people who may need that extra bit of protein are not younger gym-goers, even though this is the demographic that most immediately comes to mind when we think of protein-fortified products.
Also read: Is there an ‘ideal’ amount of protein that must be consumed?
Since the body cannot ‘store’ excess protein, it is converted to fat. Unchecked high-protein consumption can cause weight gain. This weight gain is often overlooked in the rush to ‘bulk up,’ but it underscores that more is not always better.
The kidneys and liver play a key role in breaking down and metabolising proteins. When you eat more than the body can use, nitrogen from amino acids is converted into waste products like urea and ammonia. Clearing these requires extra water, putting a strain on the kidneys and raising the risk of dehydration. Early signs include a dry mouth, dark urine, and fatigue. In people with existing kidney disease, this extra load can accelerate decline in function. Foamy or bubbly urine can indicate proteinuria (excess protein in the urine), which is often an early warning of kidney damage.
There are other ways in which protein overwhelms the body’s natural detoxification systems. The liver works harder to process excess protein, leading in rare cases to ‘protein poisoning’ where dangerously high levels of urea and amino acids build up in the blood. While extremely uncommon, it can at times be fatal.
Since the body cannot ‘store’ excess protein, it is converted to fat.
High protein intake—especially from animal sources—can also affect bone health. When protein is broken down, acids are produced in the body. To neutralise this, calcium may be leached from bones, potentially increasing the risk of osteoporosis over the long term. Research suggests that eating less protein may help lower blood ammonia levels and reduce the risk of hepatic encephalopathy—a brain condition caused by the liver not clearing toxins from the blood.
The consequences extend to heart health as well. Long-term high intake of animal protein, particularly red and processed meats, is also linked to a higher risk of cardiovascular disease, partly due to increased saturated fat, cholesterol, and elevated blood lipids. “While there’s no definite link between overall protein intake and risk of death, greater intake of animal protein is associated with a higher risk of death. And plant protein is associated with a lower risk,” says Walter Willett, professor of epidemiology and nutrition at the Harvard T.H. Chan School of Public Health.
Excess protein has also been linked to higher risks of certain cancers, especially colorectal cancer. This may be due to compounds formed when red meat is cooked at high temperatures, as well as the role of insulin-like growth factor 1 (IGF-1), a hormone stimulated by high protein intake that can promote cell proliferation.
Beyond these long-term risks, there are everyday side effects too: bad breath (due to ketones from low-carb, high-protein diets), constipation from reduced fibre intake, and gastrointestinal discomfort like bloating or diarrhoea.
Also read: Is your body low on protein? Signs and impacts of a deficiency
The Indian Council of Medical Research advises against using protein supplements as a shortcut to bulking up. Yet, protein-packed powders, shakes, and bars are often marketed as quick, convenient fixes—promising instant muscle growth, energy boosts, or weight loss. This positioning appeals to anyone looking for a faster route to fitness.
These products are often loaded with sugars, artificial sweeteners and other additives and preservatives that can undermine their supposed benefits. Excessive consumption of protein shakes or bars may also reduce your natural intake of other nutrient-rich foods, leading to a less balanced diet. If you do opt for powders or shakes, look for organic products with minimal additives and third-party safety testing, since supplement regulations are often lenient.
Protein bars, marketed as convenient fuel, can be misleading. Relying solely on them as a main protein source means missing nutrients found in whole foods: omega-3s from fish, magnesium and fibre from beans, healthy fats from nuts, and immune-boosting compounds in seeds. Nutritionists suggest sticking to one, at most two, supplemental protein servings per day—ideally after workouts or on busy days. The rest of your intake should come from varied, natural food sources, rich in amino acids essential to the body.
These products are often loaded with sugars, artificial sweeteners and other additives and preservatives that can undermine their supposed benefits.
When planned properly, Indian meals can be very protein-dense. Instead of processed powders and bars, one can opt for nutritious meals like eggs, beans, and lentil soups that can support long-term health.
Also read: Whey to go: A complete guide on protein
The latest data highlights that Indians are now eating more protein than ever–in urban as well as rural settings. In urban areas, the average person consumed 63.4 grams of protein per day in 2023-24, up from 58.8 grams in 2009-10, an 8% rise. In rural areas, the increase was smaller, from 59.3 grams to 61.8 grams per day.
Protein is essential, but balance matters. Overconsumption can burden the body and deprive you of other vital nutrients.
Protein is essential, but balance matters. Overconsumption can burden the body and deprive you of other vital nutrients. Whole, farm-fresh foods remain the best sources, and professional advice can help tailor intake to individual needs. Ultimately, the right amount depends on lifestyle, age, and health status—reminding us that protein should be seen not as a quick fix or a marketing trend, but as part of a diverse and balanced diet that supports long-term health.
Additional inputs by Harshita Kale
{{quiz}}
Born amid Chennai’s water crisis, this community took matters into their own hands, stirring bureaucrats into action
Editor’s note: The last two decades have been witness to the rapid and devastating march of unchecked urbanisation and climate change in India’s cities. Among the first victims of this change is freshwater and access to it—from rivers which sustained local ecosystems, to lakes and groundwater which quenched the thirst of residents. In this series, the Good Food Movement examines the everyday realities of neglect and pollution. It documents the vanishing and revival of water bodies, and community action that made a difference.
At the end of a 14-year-long stint in the US, in 2012, a 38-year-old techie Sunil Jayaram felt an urge to return to India—more specifically to Chennai, the city he calls home. When he set foot on Indian soil, he could not help but notice how much of urban India was drowning in waste. He was particularly struck by what was unfolding in his own backyard: the Chitlapakkam lake, situated in his neighbourhood, was choked by trash—a result of years of civil and municipal neglect. Alarmed by the decline of a public space he once held dear, Jayaram felt an urgency to act.
Chitlapakkam, a locality in south Chennai located about 25 km from the city centre, is home to nearly 60,000 residents. It urgently needed organised conservation efforts to prevent its lake from degrading beyond revival and vanishing. It all began when Jayaram identified the potential of local WhatsApp groups—meant for sharing cinema updates—to bring people together. The oft-quoted words of social activist and Nobel laureate Kailash Satyarthi, nudging people to act, echoed in his mind.
The movement’s spirit and success is also evidenced by how its neighbouring localities admire and emulate it.
He reached out to two other young Chitlapakkam residents, Udaya Utthandi and Ezhildasan. At first, their intent was focused on small-but-effective interventions: painting walls with anti-littering slogans and urging neighbours to keep bylanes and roads clean. But those small acts soon gathered momentum, growing into wider initiatives like weekend cleanups. Thus, Chitlapakkam Rising—which started a people’s movement—was born in October, 2014. To this day, it remains an active presence on Chennai’s streets and Facebook, serving as a platform for people to voice local, civic issues.
Once comprising all of three founding members, the movement has grown immensely over a decade to thousands of volunteers on the ground and followers online, driven forward by a core team of 50. After six years of consistent organising as well as strengthening the community structure and purpose, the work of the movement began to show strong results and came into the spotlight: in 2019, the Tamil Nadu chief minister earmarked Rs 25 crore for Chitlapakkam Rising’s lake restoration project. In 2024, the lake and Chitlapakkam Rising were awarded the Tamil Nadu Governor’s Award for Environmental Protection; they were recognised for designing a replicable, scalable model for urban freshwater resilience. The movement’s spirit and success is also evidenced by how its neighbouring localities admire and emulate it.

As per the National Water Bodies Census–that surveyed, for the first time, all of India’s water bodies (in 2017-18)–only about 3% of India’s 24 lakh water bodies lie in urban areas. Across the country, metros and Tier 1 cities are fast losing their water heritage. In Chennai, this erosion is especially stark: once home to more than 474 wetland complexes that supported both people and biodiversity, the city has witnessed an 85% decline–over the last three decades–in the area of its wetlands, due to unchecked urbanisation. This loss has critically affected the city’s natural ability to store rainwater, recharge aquifers, prevent floods, and manage climate-related risks.
The 2015 Chennai flood and following droughts exposed the fragility of the city’s water infrastructure, prompting renewed attention from citizens and authorities. Plenty of reports detail just how Chennai’s water bodies have been degraded by encroachment, garbage dumping, untreated sewage, and large-scale development projects; Chitlapakkam lake isn’t an outlier, but rather an example of a troubling civic reality.

In the early days of Chitlapakkam Rising, the work taken on by the founding members and volunteers involved tasks like cleaning streets and railway stations. The walls of stations were stripped of old posters and transformed with artwork. The nature of these activities attracted locals, inviting them to participate and engage. Soon, the group began to ask itself questions about the state of waste in their neighbourhood: Why was trash spilling out into public spaces? Why was its management failing? Who was responsible for it? These questions gradually shaped their collective journey from straightforward volunteerism to strong, people-driven activism.
In 2018, a catalyst came in the form of a massive garbage mound, piled over 40 feet high, beside the lake. Its stench and spillover loomed over a nearby government school, making everyday life unbearable for children and teachers alike. They reported constant nausea, vomiting, and respiratory issues due to the burning of this waste and foul smells. Even the borewell water drawn from the school grounds was reported to be contaminated. "We had to bring drinking water from outside," recalls retired school teacher Suguna Sampath.
Additionally, access to clean water became a daily struggle. Residents were paying increasing amounts for tanker water, from Rs. 600 to as much as Rs.1,500 for 6,000 litres during summers. "We used to slip into depression, waiting all day for the arrival of tankers," says Sharadha, an active volunteer with Chitlapakkam Rising.
Despite years of petitioning from 2015 to 2019, government action remained elusive—and never focused on Chitlapakkam.
This personal plight was a microcosm of an eventual citywide collapse: in June 2019, Chennai announced “Day Zero”, with all four main reservoirs—Red Hills, Cholavaram, Poondi, and Chembarambakkam—running completely dry. The whole of Chennai, especially Chitlapakkam, was hit hard, as groundwater declined sharply and access to tanker-delivered water became a matter of survival. On this day, 1.1 crore people went without drinking water.
Despite years of petitioning from 2015 to 2019, government action remained elusive—and never focused on Chitlapakkam. It was only when the citizen movement grew and drew larger public attention that the bureaucrats stepped in. "We decided to desilt the lake ourselves. When we did, 1,500-2,000 people joined us. That pressure made the government act," says Jayaram.

The local community was moved to act, even as bureaucratic processes moved at their own pace. Driven by a shared purpose to revive their neighborhood lake and its surroundings, a group of informed and determined residents, including engineers, IT sector workers, climatologists, retired government employees, and homemakers, came together to form a collective that continues to highlight the community’s efforts and spirit. Udayavaani, a civil engineer from the neighbourhood, explains, “The challenges we collectively faced brought us together and after the floods, it became clear that no one was coming to help. We had to take matters into our own hands.”
Social media became a powerful, vital tool during times of crisis, helping the residents to mobilise, put pressure on officials, and draw in volunteers. As a well-informed and closely knit community, they turned to social media to organise, amplify their voices, and demand attention. With relentless posts tagging officials and visual evidence in their hands, the community made it impossible for the government to ignore their plea. As a result, in 2019, the government sanctioned Rs 25 crore under the Water Resources Department (WRD) for the lake’s restoration—a milestone for Chitlapakkam Rising.
The WRD’s Assistant Engineer Narendrakumar, who led the restoration, praises the community’s knowledge and commitment, highlighting that daily petitions poured in not just from groups, but individuals, too.
Also read: Bengaluru is fated to run out of water. When will the crisis hit?

Experts agree that there is no universal approach to restoring water bodies. Each lake or pond has its own set of challenges and must be understood within its specific ecological, social, and cultural context. For this reason, every restoration project begins with a detailed assessment. During this phase, teams study crucial aspects such as water flow patterns, hydrological conditions, and soil quality. Geospatial mapping and climate analysis are also conducted to identify peak water levels and understand seasonal variations.
“Before we began the full-fledged restoration, we decided to approach the problem scientifically,” says Dayanand Krishnan, a civil engineer and a GIS consultant from the community. Many other members–like Krishnan–from the community were mobilised by Chitlapakkam Rising wherever they were needed: for legal processes, political efforts and greening projects. Krishnan, on his end, proposed installing a gate system at all of the lake’s inlets to prevent the entry of sewage water—a first-of-its-kind approach for an urban lake in Tamil Nadu. This would control the inflow and redirect the sewage; a collection well on the southern side of the lake would divert the wastewater away from the main waterbody. The idea was later adopted by the WRD, which eventually designed and implemented the model.
Generally, in urban setups, sewage from homes flows through 6-inch pipelines into manholes, which then transport the waste to pumping stations–essentially, to large underground wells. From there, it is either treated or directed to larger bodies like rivers or lakes.
"The lake was no longer just water storage; it was climate adaptation in action," says Kumaran Ram, a volunteer climatologist involved in the planning.
In the Chitlapakkam model, the lack of visibility in stormwater drains was addressed: when the cover slabs over these drains break or go missing, it becomes difficult to detect whether sewage is mixing with stormwater.
“Another innovation was the way this system helps dry the lake during summers, allowing any residual black water to be drained. This drying period makes it easier to remove siltation. Silt forms a layer that prevents rainwater from percolating into the ground. Think of it like a layer of soap blocking water flow in a bathroom drain; silt does the same to soil, blocking groundwater recharge. By controlling sewage inflow and regularly removing silt, we ensured the lake could breathe again, literally and hydrologically,” says Krishnan.
“Trial pits were dug up to 10 feet to assess soil permeability. Soil samples were tested by PWD labs, confirming that effective recharge was taking place beyond 6 feet. This scientific approach is essential for building climate resilience,” Narendra explains.
Chitlapakkam lake’s original storage capacity was around 7 million cubic feet, but years of neglect had reduced it to just 5 million. The desilting process, along with proper deepening and strengthening of bunds, didn’t just bring the lake back to its former state; they significantly enhanced it. Today, the lake can hold up to 12 million cubic feet of water, storing rainwater during monsoon and supplying it during summer.
For a lake to aid in water conservation and flood mitigation, it must turn dry during summers and absorb water during monsoons, rather than overflowing. The renewed rainwater harvesting capacity in Chitlapakkam was built to withstand 60 cm of rainfall, inching closer to Chennai’s average of 100 cm. "The lake was no longer just water storage; it was climate adaptation in action," says Kumaran Ram, a volunteer climatologist involved in the planning.
Also read: The intertwined fate of Navi Mumbai’s Kolis and the Kasardi river

Creating walkways, parks, and pathways around a lake can instill a sense of ownership among the youth. "Other lakes around Chennai have started adopting a similar model," says WRD Assistant Engineer Narendrakumar. Such transformations can fill the community living nearby with pride. “During our early postcard campaigns (a movement circulating informational material, collecting signatures), the children themselves pointed to this dumpyard and collected signatures demanding its removal. Today, as we stand in this transformed space, those memories make the journey feel even more meaningful,” says Udayavaani.
“People once called this area ‘Kuppamettu School’ (a school near a garbage settlement) and ‘Saakada Eri’ (a lake turned into a dumping ground)—names that reminded us of how neglected this place used to be. But now, when someone says Chitlapakkam, they talk about the beautiful lake here, and that change fills me with pride”, says Suguna.
However, the construction of a sewage treatment plant (STP) is yet to be initiated by the local government, which leaves the question of long-term success that lasts generations, unanswered.
Also read: In Gurugram’s rise, a cautionary tale about satellite cities and groundwater

“For any institutional change, classifying all urban water bodies as hydro reserves—akin to reserve forests—would help in their maintenance and make people and governments accountable for any illegal activities taking place in their vicinity,” says Arun Krishnamurthy, the founder of Environmentalist Foundation of India which works across the country for wildlife conservation and habitat restoration. “A multi-stakeholder task force should be created with representatives from the judiciary, government, academia, and local organisations, to keep a check on dying water bodies that can be rejuvenated."
There’s also a need to change public perception: lakes should not be seen merely as recreation zones or flood buffers, but as ecosystems that need biodiversity to thrive. "We all want the lake to be ‘comfortable’ for us. That’s the wrong mindset. Instead, we must think from nature’s perspective," says Ramaswamy, a concerned Chitlapakkam Rising volunteer.
"We all want the lake to be ‘comfortable’ for us. That’s the wrong mindset. Instead, we must think from nature’s perspective," says Ramaswamy, a concerned Chitlapakkam Rising volunteer.
Members of the movement are now extending their support to nearby localities, such as Sembakkam and Nanmangalam, where pressing issues include sewage mixing into the lakes and the rampant growth of water hyacinths, which clog water flow and damage the water table. Alongside their weekly clean-up and maintenance drives within Chitlapakkam, they help other groups by guiding them in filing petitions and raising awareness.
What initially emerged as collective knowledge and learning within one movement, one neighbourhood, has evolved into a sustained, community-driven process—one that thrives on follow-ups, demanding accountability, and a commitment to long-term change. This model of solidarity underscores the power of individuals coming together, not just to clean but to transform. As India faces the escalating twin crises of urban water and waste, the success of Chitlapakkam Rising shows that solutions lie not only in government policy, but also grassroots action. When informed citizens take charge, change becomes not only possible, but inevitable.
Artwork by Prabhakaran S
Edited by Neerja Deodhar and Anushka Mukherjee
Produced by Nevin Thomas and Neerja Deodhar
{{quiz}}

Traditionally, India processed foods through pickling and fermenting. Industrially produced, packaged foods are markedly different
The Plate and the Planet is a monthly column by Dr. Madhura Rao, a food systems researcher and science communicator, exploring the connection between the food on our plates and the future of our planet.
Walk into any grocery store today, and you're likely to find shelves stacked with shiny packets, instant mixes, and colourful snacks that promise taste, speed, and convenience. From breakfast cereals to frozen parathas, ultra-processed foods (UPFs) have become a staple of modern life, especially in urban India. But behind the vibrant packaging and clever marketing lies a more complex story about convenience and its consequences: what exactly are these foods, how did they become so ubiquitous, and what are the effects of their growing presence in our diets?
The term ‘ultra-processed food’ was introduced in 2009 by Brazilian nutrition researcher Carlos Monteiro, who also developed the NOVA classification system. Now widely used in global debates on food and health, this system groups foods into four categories based on the extent to which they have been processed.
At one end are unprocessed or minimally processed foods, such as fresh, dried, frozen or fermented fruits, vegetables, grains, milk, eggs and meat. Next are processed culinary ingredients like oils, ghee, sugar and salt, which are extracted from whole foods and used in cooking. The third category includes processed foods such as cottage industry-produced foods, like papads, pickles, and fried snacks, made by combining foods from the previous two categories. The final category is ultra-processed foods, which are industrial products made mostly with refined ingredients, often with little or no whole food content and with multiple additives. These are designed for convenience and wide appeal, and are usually marketed aggressively. Biscuits, sausages, heat-and-eat meals, vanaspati (hydrogenated vegetable oil), and infant formula are typical examples.
I find that the older colloquial term junk food does a better job of capturing the problem.
The logic behind NOVA is that the more a food is transformed by industrial processes, the more likely it is to contribute to poor health. And there is growing evidence to support this idea. Numerous studies have shown that diets high in UPFs are associated with a greater risk of obesity, heart disease, type 2 diabetes, gastrointestinal issues, and even certain cancers.
However, the term ‘ultra-processed’ and the NOVA categorisation itself, are not without problems. Critics have argued that the problem with UPFs isn’t necessarily how they’re made, but rather their poor nutritional quality: high in sugar, salt, and unhealthy fats, and low in fibre and micronutrients like vitamins and minerals.
A colleague who teaches food engineering recently offered a useful example. He explained that plain yoghurt falls under NOVA category 3, processed foods. But add a swirl of fruit jam or artificial flavour, and it moves to category 4, ultra-processed. The change in processing is minimal. In an industrial setting, it may be as simple as opening an extra valve to add ingredients. Nutritionally, though, the difference is more significant. Flavoured yoghurt often contains added sugar, colour, and other substances that alter its health profile, even if the underlying process remains pretty much the same.
The current wave of industrially produced and packaged foods marks a distinct departure from traditional processing in both method and purpose.
I find that the older colloquial term junk food does a better job of capturing the problem. It points more directly to the nutritional quality of the food, rather than how many industrial steps went into making it. Although a sugary soft drink and packaged buttermilk fall into the same NOVA category, the former is ‘junk’ while the latter is not, owing to their very different nutritional profiles. That said, it is also important to recognise that while processing itself isn’t inherently harmful, industrial food processing often enables and amplifies nutritional risks. The very features that make UPFs appealing—long shelf life, hyper-palatability, and low cost—are achieved by manipulating ingredients in ways that tend to skew their nutritional profiles. In this sense, the process can’t be separated from the product: the way something is made often dictates what kind of food it ends up being. Therefore, for the purpose of this column, I will use ultra-processed foods to describe industrially manufactured unhealthy food products, even as I remain cautious about the limitations of the term.
Also read: Protecting place and power, not people: The trouble with GI tags
Ultra-processed foods have become an increasingly prominent part of the Indian diet in recent decades. While traditional Indian cuisines have always included some forms of processing, such as fermenting, drying, pickling, and roasting, these techniques were typically used for preservation, flavour enhancement, or out of seasonal necessity. The current wave of industrially produced and packaged foods marks a distinct departure from traditional processing in both method and purpose.
Today, ultra-processed foods are available almost everywhere in India, from village shops to railway stations, typically at low price points and in highly portable formats. According to a 2023 WHO report, their retail value jumped from just USD 0.9 billion in 2006 to over USD 37.9 billion by 2019, and they are projected to make up nearly 39% of all processed food sales in the country by 2032. Between 2011 and 2021, chocolate and confectionery accounted for the largest share of retail sales, followed by ready-to-eat foods. Beverages held the third spot for much of the decade, but by 2021 they were overtaken by salty snacks.

A major shift in Indian diets began with the liberalisation of the economy in the early 1990s. The entry of multinational food corporations, along with the rapid growth of domestic food industries, brought a wide range of new products into the market. Instant noodles, processed cheese, mass-manufactured snacks, and breakfast cereals became increasingly common in urban households. Designed for convenience, affordability, and consistency, these foods aligned well with the needs of a population that was becoming more urbanised, time-constrained, and influenced by globalised ideals. As more people moved to cities and more women—typically tasked with cooking and carework—entered the formal workforce, traditional cooking practices became harder to sustain. Packaged foods that required minimal preparation offered a practical solution, while advertising campaigns framed them as modern and aspirational, tapping into middle-class values around hygiene, efficiency, and a globalised lifestyle.
Over the years, UPFs started appearing in school lunchboxes (cold Maggi nostalgia, anyone?), office tiffins, evening snacks, and even festival offerings. Many traditional foods started to be re-engineered for mass production, with ingredients adjusted to suit long-distance transport and extended shelf life. These changes often go unnoticed by consumers, as familiar names and packaging maintain the appearance of tradition, even when the contents and production methods had significantly changed. Brands which began as family-run businesses serving freshly prepared foods to local customers, have expanded into large-scale manufacturers, leveraging their brand value as familiar household names to market packaged versions of their products for mass markets in India and abroad.
Also read: What it takes to feed India’s growing cities
While most research and debates on UPFs have focused on health risks, their environmental impact is increasingly coming into view. UPFs rely heavily on a narrow set of monoculture crops like maize, soy, wheat, and oil palm, that reduce biodiversity, degrade soil, and pollute water. Animal-based UPFs often depend on intensive livestock systems that contribute to deforestation and carbon emissions. Beyond farming, UPFs require energy-intensive industrial processing, extensive plastic packaging, and long-distance transport, all of which add to their environmental footprint. Yet most assessments overlook these broader ecological costs, focusing only on farm-level production.
Multinational food corporations also often engage in greenwashing. For example, a snack may be advertised as ‘eco-friendly’ because of its packaging, while its large scale and cheap production was enabled by energy-intensive processing or extractive use of natural resources.

In India, the conversation about regulating ultra-processed foods is a very recent one. The Food Safety and Standards Authority of India (FSSAI) has yet to introduce regulations that directly address the marketing, composition, or availability of UPFs. For a long time, the absence of formal definitions was cited as a reason for inaction. That changed recently when in 2024, the Indian Council for Medical Research (ICMR) and the National Institute of Nutrition (NIN) released updated dietary guidelines. These guidelines offer a clear definition for UPFs and link their consumption to rising rates of obesity, diabetes, heart disease, and other non-communicable illnesses. Public health experts have since called for immediate regulatory action.
UPFs rely heavily on a narrow set of monoculture crops like maize, soy, wheat, and oil palm, that reduce biodiversity, degrade soil, and pollute water.
The same guideline also introduced ‘HFSS foods’, a category referring to products high in fat, sugar, or salt. Public health groups are now pressing the FSSAI to strengthen front-of-pack labelling by requiring warnings on HFSS products. Since most packaged foods high in fat, salt, or sugar are also ultra-processed, this approach could serve as a first step toward meaningful UPF regulation. Yet progress has been slow. The FSSAI missed its July 1 deadline for updating food labelling rules, and the Supreme Court has given the regulator three more months to submit recommendations.
In many other countries like Chile, Peru, Brazil, the UK, and South Africa, governments have introduced fiscal and regulatory measures such as taxing UPFs, restricting their marketing, and mandating warning labels. Most of these strategies aim to shift consumer behaviour, operating on the assumption that food choices are largely a matter of willpower or awareness. While such measures have had some impact, UPF consumption remains a significant public health challenge worldwide. India should take note of these limitations and proceed with caution as the country’s food regulators move to rein in the spread of UPFs.
In most Indian homes, the responsibility for daily cooking, grocery shopping, and meal planning still falls largely on women. Even as more women take on paid work outside the home, they continue to manage the bulk of tasks related to feeding the family. The rise of UPFs has not eliminated this burden, but it has made it more manageable. Instant mixes, packaged snacks, and ready-to-eat products have allowed many women to meet their family’s food needs while juggling long hours of work and other domestic obligations. If UPF consumption is discouraged without offering affordable, time-saving, and nutritious alternatives, the burden of daily food preparation could intensify; falling disproportionately on women and deepening existing gender inequities. Blanket labelling of all ultra-processed foods as harmful risks unfairly confusing consumers and adding to the cognitive burden of preparing meals that are both nutritious and time-saving.
If UPF consumption is discouraged without offering affordable, time-saving, and nutritious alternatives, the burden of daily food preparation could intensify; falling disproportionately on women and deepening existing gender inequities.
If the negative health impacts of UPF consumption are to be addressed meaningfully, corporate accountability must be central to the reform. In many developing countries with weak regulatory frameworks and unchecked privatisation, multinational food companies often sell products of significantly lower nutritional quality than those marketed in higher-income countries. To prevent this disparity, governments must intervene and make it mandatory for manufacturers to meet strict nutritional standards. Setting upper limits on salt, sugar, and saturated fat, requiring full disclosure of ingredients, and restricting the marketing of unhealthy products would help shift the burden of responsibility from individual consumers to the corporations that shape the food environment.
At the same time, the state has a vital role to play in expanding access to healthier alternatives through public infrastructure. Strengthening schemes such as the mid-day meal programme, anganwadi services, and meals served in public institutions can improve access to nutritious, minimally processed food. These initiatives should be designed not only to meet dietary requirements but also to reflect cultural food practices and ensure that healthy eating is both accessible and acceptable across diverse communities.
Yes, but not just about the foods themselves. The real concern lies in the larger systems that make ultra-processed foods so widespread in the first place. Addressing their health and environmental risks means going beyond personal choice to rethink food policy, corporate accountability, and the unequal conditions under which people make food-related decisions. A healthier future will require not only changing what’s on our plates, but also reshaping the structures that decide what ends up there.
Artwork by Alia Sinha
Also read: The promises—and perils—of Indian aquaculture
{{quiz}}

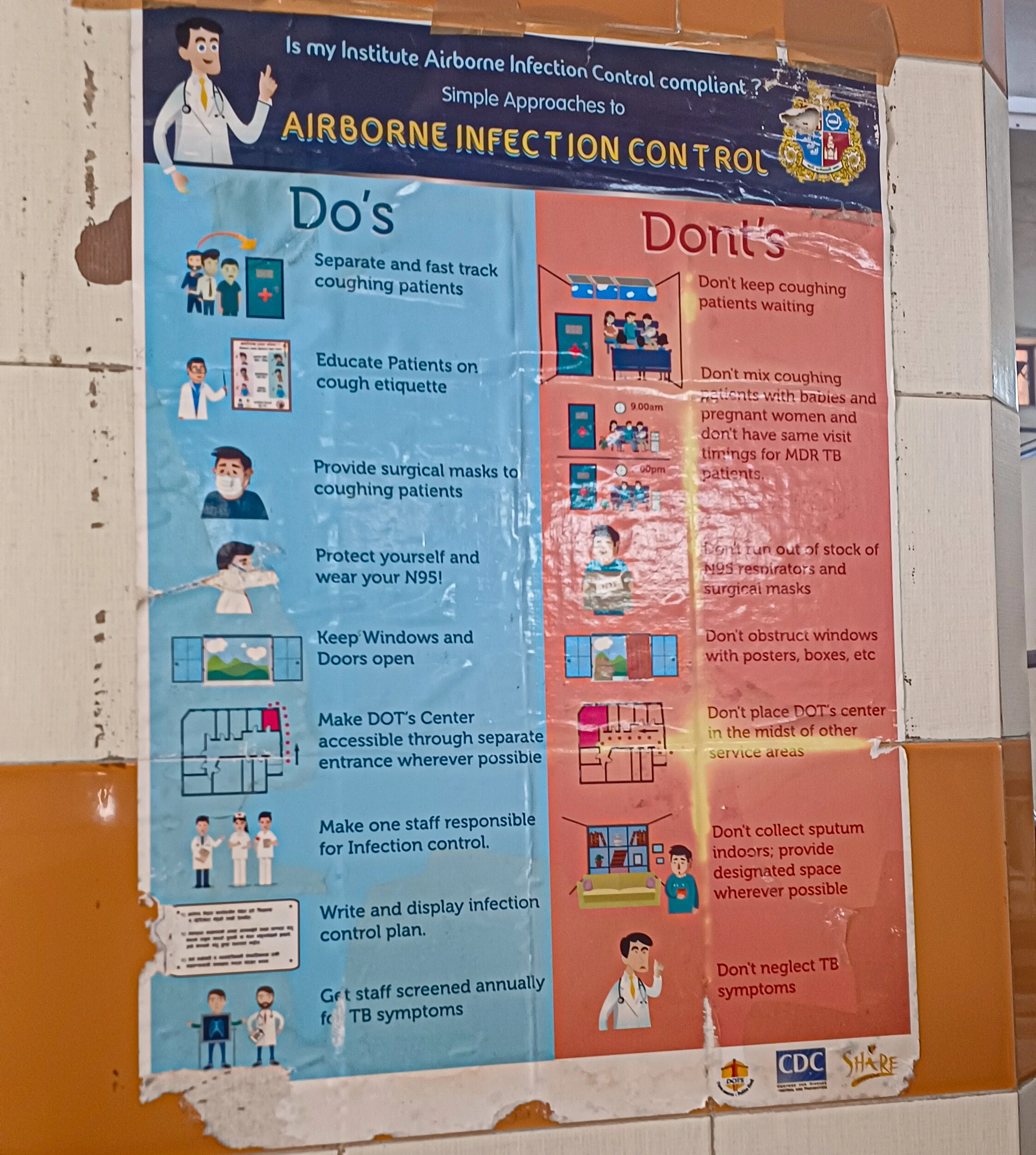
Lack of adequate nutrition increases vulnerability to TB and prolongs recovery from it
At a government-run tuberculosis (TB) hospital in Mumbai’s Malad suburb, 29-year-old Usha and her mother wait patiently for their turn to get medicines. Uma, who is 50, was diagnosed with Drug-Resistant Tuberculosis (DR-TB) a week ago at a private clinic. She wears a weary look on her face.
"I have been coming to this hospital for three days for these medicines, leaving my work aside—with no doctor in sight. My mother's condition has worsened over a week, with a persistent cough and fever due to delayed treatment," Usha says.
At another government-run hospital in the nearby suburb of Kandivali, frail-looking, 40-year-old Ashok—the sole breadwinner of his family of three—waits. Diagnosed with TB nearly seven years ago, he now fears a relapse. “I was coughing heavily and unable to breathe when I was first diagnosed. I completed my treatment and recovered, but recently, I have begun experiencing chest pains again and fear that a relapse is imminent."
In 2018, the Government of India launched the Nikshay Poshan Yojana to provide monthly monetary assistance of Rs. 500 to TB patients for adequate nutrition through centralised Direct Benefit Transfers (DBT). The amount of the aid was raised to Rs. 1,000 earlier this year. At the time of the scheme’s launch, Ashok—the resident of a small tenement in Mumbai—didn’t reap any of its benefits because he was unaware about the Yojana. And though he received timely medication from the government hospital, managing his nutrition as per the doctor’s advice was challenging, as both his wife and son depended on him. He believes that the government should provide sufficient financial assistance and rations to patients suffering from the disease.
Globally, India leads in DR-TB with 1,35,000 cases of MDR/RR TB annually due to a lack of rapid diagnoses in low-resource settings, posing a significant constraint on DR-TB treatment.
Many vulnerable socio-economic populations in India, especially informal and migrant workers, are unable to afford the luxury of rest and proper nutrition without remaining reliant on daily wage work. This is despite schemes like the Nikshay Poshan Yojana, as patients in need remain unaware about their provision.
The United Nations defines TB as a bacterial infection primarily affecting the lungs, but it can also affect the brain and spine. It is caused by the Mycobacterium tuberculosis bacteria. The World Health Organization states that India has the highest number of TB cases worldwide; the country reported 26.07 lakh tuberculosis cases in 2024, with Uttar Pradesh reporting the highest cases at 6,81,779, followed by Maharashtra at 2.25 lakh cases. Mumbai contributed 60,051 cases to the state's numbers in 2024.
The death rate from multidrug-resistant TB (MDR-TB), specifically, hovers around 20% in India—higher than the global average of 17%. These figures depict dire on-ground realities; for context, the National Tuberculosis Elimination Programme (NTEP) aimed to eradicate TB by 2025, five years ahead of the Sustainable Development Goals (SDGs) target of 2030.
| Types of DR-TB | |
|---|---|
| Mono-resistance | Resistance to a single first-line anti-TB drug (medication which is given when TB bacteria is susceptible to the medicine) |
| Poly-resistance | Resistance to more than one first-line drug, excluding both isoniazid and rifampicin |
| MDR-TB | Resistance to both isoniazid and rifampicin |
| XDR-TB | MDR-TB plus resistance to a fluoroquinolone and at least one of the second-line (drugs used when resistance is developed to first-line drugs, or when patients cannot tolerate them) injectable drugs, such as kanamycin, amikacin, or capreomycin |
The different types of DR-TB are mono-resistant, poly-resistant, MDR-TB, and extensively drug-resistant TB (XDR-TB). Around 3.2% of new DR-TB cases are MDR-TB/rifampicin-resistant—they resist first-line drugs, or the first round of drugs that is administered when the bacteria still responds to medication. When the bacteria resists this first round, like in the case of DR-TB, the infection is fought with a different combination of medicines: second-line drugs, which can be more toxic, more expensive and less effective.
Globally, India leads in DR-TB with 1,35,000 cases of MDR/RR TB annually due to a lack of rapid diagnoses in low-resource settings, posing a significant constraint on DR-TB treatment. As a result, it is estimated that around 56% of MDR-TB cases remain undiagnosed in India.
The WHO guidelines recommend using rapid molecular tests like GeneXpert to diagnose DR-TB instantly, offering detection in less than two hours, compared to conventional culture-based methods, taking several days or weeks. However, these services are scarce in the rural hinterlands of India, especially the Northern states.
Only one in three DR-TB patients worldwide receive high-quality care, the WHO notes. In India, which contributes over 27% of global cases, DR-TB presents a significant public health problem, as patients often require changes in their treatment plans, usually linked to poor treatment adherence in peripheral and resource-limited zones. Drug-resistant tuberculosis cases increased by 36% in Mumbai between 2015 and 2017.
In 2022, the WHO recommended using a shorter six-month regimen called BPalM, consisting of four drugs, to treat DR-TB—compared to the standard 18-24 month regimen—as it has a global success rate of 85%. This positive statistic comes with better treatment outcomes, reduced mortality rates and less infectiousness in recovery. BPalM is also significantly more cost-effective—and the reduced treatment costs ensures more access to patients.
However, India has adopted this regimen conditionally, and private practitioners don't have access to prevent its misuse. In Mumbai, a hotspot for drug-resistant TB, only 144 patients have been given the BPalM regimen this year on a pilot basis.

Also read: Antibiotic overuse is turning your gut against you
There are several types of TB. It can be inactive (latent TB): the infected individual does not have symptoms and cannot spread the infection, which is suppressed by treatment. It can be active: the infected individual can spread the infection through droplets in the air.
Active TB can be treated and even cured, but it is a particular kind of active TB that scares doctors and patients alike: the forms that are drug-resistant, meaning one or more anti-TB drugs administered to the patient show no effect on the bacteria. It fights back.
Dr. Indu Bubna, a Mumbai-based pulmonologist with over 20 years of experience, says, "DR-TB is a form of TB that does not respond to the primary anti-TB drugs, particularly isoniazid, and rifampicin because of incomplete or incorrect treatment. DR-TB is more toxic and requires lengthier treatment." According to Dr Bubna, the challenge emerges when a patient is diagnosed with XDR-TB (extensive drug-resistant TB)—a more severe form of DR TB—making the case more complex with the failure of second-line drugs.
Though India is widely considered the ‘pharmacy of the world’, TB patients in the country suffer due to the lack of medicines.
"In India, before visiting a government Directly Observed Treatment (DOT) centre, patients tend to self-medicate, delaying diagnosis. Often, treatment is started based on X-rays without the appropriate tests because of strained finances," Dr Bubna adds. Drug shortages during the patient's treatment can also cause interruption, making the disease more resistant.
TB is known as the "disease of poverty" because the chances of contracting it are furthered by factors such as malnourishment as well as the lack of air and sunlight in cramped residences. An airborne disease, it is caused only by inhaling infectious droplets from the air. TB is not caused by any changes in diet, or anything in the water, but these are still really important factors in the context of the disease. Malnutrition renders the immune system weak; a malnourished person is more at risk to get infected by TB—in fact, it increases the risk by 13.8% per unit decrease in the body mass index (BMI). The body’s ability to respond to treatment is severely affected, as poor nutrition can prolong recovery. Moreover, some people develop resistance to TB over time, and this can be due to the lack of access to proper nutrition and prescribed, timely dosages.
Malnourishment is also a risk factor in converting latent TB to active TB, and this weakness in immunity also makes patients less likely to recover once they do contract the disease.
Dr Bubna points out that the incidence of TB is now increasing in the middle and higher income sections of India’s population as a result of one specific reason: these sections follow rigid, traditional diet regimens that are often lacking in nutrition. "TB is not just about malnourishment—it also manifests in patients who don't eat food on time and travel in overcrowded spaces. Furthermore, people with HIV, diabetes and those who indulge in drug abuse are also vulnerable," says Dr Bubna.
Malnutrition renders the immune system weak; a malnourished person is more at risk to get infected by TB—in fact, it increases the risk by 13.8% per unit decrease in the body mass index (BMI).
The prevalence of TB can be linked clearly to a lack of access to nutrition as well as a flawed approach to nutrition. Dr. Bubna explains, “While the Public Distribution System (PDS) and mid-day meal programs provide calories and iron-fortified staples like rice and atta, these diets often lack adequate protein and key micronutrients. Protein is especially important because it helps rebuild tissues, strengthen muscles, and restore immune function. Micronutrients such as zinc, vitamin D, vitamin A, and B-complex vitamins are also vital for immune defense and healing, but these are often missing in the diets of TB patients.” The gap lies in the difference between calorie sufficiency and nutrient adequacy: patients often get food that satiates hunger, but does not provide the quality of nutrition required for faster recovery and reduced relapse risk.
"In India, most people lack either vitamins B12 and D, or protein,” Dr. Bubna points out. This is also reflected in the burden of disease that India carries: we account for around 27% of TB cases across the world. A well-balanced diet rich in proteins and vitamins, like iron, zinc, B12, and D3, is essential for patients battling DR-TB. Addressing TB care's social and nutritional loop is essential for its elimination.
According to government data, over Rs. 3,200 crore have been disbursed to 1.13 crore TB patients under the Nikshay Poshan Yojana; the government has committed another Rs. 1,040 crores as a 60:40 divide between the centre and states, under the same programme.
The unaffordability of nutrition is a concern for several patients in India. Even with low prices, a healthy diet remains out of reach for nearly 74% of Indians, according to a UN agency report. "Doctor sensitivity also plays a crucial role in wholesome counselling. Without that, the prescription is never complete. Every TB patient should have a protein and iron-rich diet, comprising green leafy vegetables, one fruit, paneer, soya, and several proteins, because they have a high risk of relapse and mortality for DR-TB."
Also read: The warning about antibiotics we should have heeded
To improve diagnostic services, says Dr. Bubna, governments must decentralise testing, improve sample transport, and integrate private labs into the national network—changes that are underway in Mumbai. However, India’s more remote centres lack even basic tests like the Line Probe Assay (LPA), a quick molecular test that presents results within 24–48 hours.
Screening and testing for TB early and accurately is extremely crucial to treatment and recovery from this infection, and there are multiple provisions in place for this. In 2012, the Government of India made TB notification mandatory for both public and private sector healthcare providers. In 2017, the Government of India announced a National Strategic Plan (NSP) to eliminate TB, and set aside a budget specifically for testing. The very next year, the Ministry of Health and Family Welfare issued another order stating that doctors, pharmacists, chemists, and laboratory staff could face jail time if they fail to notify TB cases.
Despite these stringent rules, India contributes approximately 25% of “missing” TB cases globally, as the WHO estimates that approximately 1 million TB cases in India are not recorded annually. A detailed report from IndiaSpend reveals that while the NSP aimed to spend funds on diagnostic equipment, testing kits, and increasing testing in the private sector, they only spent “2.1% of [their] budget (Rs 4.34 billion) on diagnostics up to 2023-24.” While the 100-day campaign to eradicate TB introduced by the centre in 2024 did amp up testing and diagnosis in several states, the overall practice remains uneven in the country. In some places, testing facilities are either defunct or non-existing, like in Haryana—where the only state-level laboratory closed due to lack of support staff—or districts in Bihar, where none existed until 2020. As a result, it is estimated that around 56% of MDR-TB cases remain undiagnosed in India.
Even delayed results of testing pose a threat for this precarious disease. Public health activist and TB survivor Ganesh Acharya draws attention to how delays in test results, even for basic investigations like X-rays, can have negative consequences. "Referrals by doctors at government-run hospitals require a 15-day window to provide services like CT and MRI, making the initial stage more painful for patients with significant out-of-pocket expenditures. Ideally, test results should be available in two hours through the Cartridge-Based Nucleic Acid Amplification Test (CBNAAT).” CBNAAT is a rapid molecular diagnostic test used to detect TB, which promises quicker results because it’s a fully automated test that analyses DNA from sputum samples. “However, the lack of resources and the staff makes the provision challenging.” Acharya adds.
Despite these stringent rules, India contributes approximately 25% of “missing” TB cases globally, as the WHO estimates that approximately 1 million TB cases in India are not recorded annually.
According to Firoz Shaikh, the general district supervisor for Mumbai's TB department, "The testing facilities for the GeneXpert test—a type of CBNAAT test—are available for free in government hospitals like the Sewri Hospital, Topiwala Hospital, and Shatabdi Hospital in Mumbai." Yet, a glaring concern is that the government department only contacts patients seeking private treatment to complete their treatment on time—a provision largely missing for patients in government-run hospitals, according to Shaikh.
"Usually, patients from higher income groups don't register on the Nikshay portal for the government's DBT transfers. Sometimes, patients receive Rs 1000 monthly for their treatment, but there are times when the amount is released later. To resolve this, patients can download the Nikshay Mitra application and complain using the toll-free number." Shaikh adds that the Nikshay schemes have been relatively successful in Maharashtra compared to other states in India. "The patients respond regularly to avail these schemes in Maharashtra as the diagnosis rate is higher."
Public health activist Acharya rues the lack of accountability within the public sector. “The Nikshay Poshan Yojana is a centralised Direct Benefit Transfer (DBT) scheme; I don't understand the reasoning behind delays in payments. Furthermore, I have heard of cases where individuals have received only Rs 500 (half of what they ought to have received).” These gaps are glaring, especially when we consider that a trial held in the states of Odisha and Jharkhand found that adequate food packages given to patients significantly improved their health outcomes.
Challenges in testing and monitoring only add to the financial and emotional burden caused by drug shortages. Though India is widely considered the ‘pharmacy of the world’, TB patients in the country suffer due to the lack of medicines. For instance, essential treatment drugs are unavailable for months in states like Uttar Pradesh. In 2023, a Times of India report found that Pilibhit in Uttar Pradesh was facing a drug shortage, unable to provide for approximately 1,200 frontline TB patients, including 124 MDR-TB patients.
"Skipping a dose on even one day is a big mistake for a TB patient, but there is nothing one can do when the government machinery runs out of medicine. This is a very negative aspect of the program, as it fails to address the systematic gaps for essential medicines," says Acharya.

Dr. Bubna steers the conversation back to patients: understanding the importance of nutrition at home and within families is essential. Immediate digital awareness, volunteers—such as those under the Nikshay Mitra scheme, where people adopt TB patients to aid them with nutrition support until their recovery—as well as the integration of community kitchen services for those without houses or migrant DR-TB patients, the presence of counsellors at clinics—all represent crucial, effective interventions that make patients cognizant of the role nutrition plays in their ailment.
"In rural areas, anganwadis and caregivers can work together to ensure food security, with the availability of fortified food rich in iron, folic acid, and vitamins. If supported with proper nutrition like probiotics and proteins, the side effects of drug doses can be mitigated."
Mehra adds that schemes like the Nikshay Poshan Yojana have made a significant difference but are inadequate in a country where a high-protein diet is costly.
According to Acharya, urban areas like Mumbai’s Govandi suffer more due to a lack of basic provisions such as sanitation and proper ventilation. "The fight is not just about a 100-day awareness campaign. It has to be systematic, with measures like food, sanitation, and open spaces. Political will has to be informed by survivor consultations."
According to Chapal Mehra, a public health practitioner and founder of the forum Survivors Against TB, "Nutritional provisions play an essential role in health security. Those affected by TB tend to belong to the lower-middle class and middle class, and often, the person who is affected is also the primary breadwinner of their family.”
Mehra adds that schemes like the Nikshay Poshan Yojana have made a significant difference but are inadequate in a country where a high-protein diet is costly. "What can one get for Rs 1,000? We can't say that the government is not trying, but it's not enough, and the amount under the Yojana should be increased to Rs 2,000 for basic provisions."
With inputs from Sijal Sagarika
Also read: Meet the minds investigating bugs lurking in poultry
{{quiz}}

From housing societies, to hospitals, to temples, composting is having its moment in the sun
Editor's Note: In this series, the Good Food Movement explores composting—a climate-friendly, organic way to deal with waste. We answer questions about what you can compost, how to build composting bins and how this process can reshape our relationship with nature and our urban ecosystem.
Every small action we take creates ripples in a larger chain of change—whether it’s rethinking what we eat or how we confront the waste our cooking leaves behind. Too often, that waste becomes someone else’s burden, carted away to landfills in urban and rural spaces alike, already overflowing with trash.
But there’s another way. Through regenerative practice like composting, what seems like waste can be reused and returned to the earth. Even in cramped spaces, all it really takes is a bin and patience. And when people come together, the impact multiplies. From housing societies in Mumbai to individuals inspiring entire communities in Bengaluru, composting has helped turn everyday scraps into rich nourishment for the soil—nurturing potted plants, neighbourhood gardens, and local trees.
Green Garden Apartments, a 73-bungalow community in Chembur in suburban Mumbai once sent 600 kg of mixed waste every month to landfills. In 2018, the apartment complex embraced zero-waste living, segregating waste and composting organic content to produce 100 kg of compost each month. At Silver Crest, Powai, residents process organic waste onsite, using compost for landscaping and donating the surplus to farmers.
In Bengaluru’s Mantri Paradise complex, housekeeping staff now spend a couple of hours each day tending to aerobins that transform used tea leaves, fruit peels, and vegetable scraps into 60 kg of rich, earthy compost. This has led to monthly savings of roughly ₹15,000 on manure purchases and the elimination of foul odours, all thanks to twelve community-installed composters and diligent waste segregation.
Also read: Can composting be the solution to expanding landfills in cities like Bengaluru?
Even the country’s temples are changing their relationship with waste. In Mumbai, the Shree Parleshwar and Mahalakshmi temples pack offerings of marigold and jasmine into boxes of culture mix, producing compost in three weeks. In Tamil Nadu, the Mission Sunehra Kal initiative has 182 temples transforming their floral offerings into rich manure for their own gardens.
Educational institutions are increasingly prioritising waste management as well. Organisations such as the Vivekanand Education Society, Guru Nanak Khalsa College of Arts, Science and Commerce, and Ashoka University, along with several schools and hospitals in cities like Pune and Bengaluru, have launched initiatives to responsibly manage their waste. Hospitals too—such as Cooper Hospital in Mumbai and the Artificial Limb Centre in Pune—have begun composting efforts to handle their waste more sustainably.
Additionally, numerous individuals are experimenting with composting in their own homes and communities, showing that it doesn’t take much to get started. No matter what the scale, their efforts prove that composting can fit into any lifestyle.
After retirement, Rajinder Singh turned to terrace gardening. When his plants initially failed, instead of hiring help, he learned plant care himself. Today, his lush rooftop boasts over 500 plants—fruits, vegetables, and flowers—all nourished by the 100 kg of compost he produces from household waste.
Faced with waste piling up in mounds outside her Khagual home, Kumari embraced a sustainable waste management program in 2017. She began composting kitchen scraps, growing her own produce, and reusing containers. Her leadership inspired 350 households to adopt composting, cutting open dumping by 60% and creating cleaner, safer streets.
Starting small, Sohoni learned how kitchen waste could become a resource. He introduced composting to his 220-unit housing society, converting 72 tonnes of organic waste. In 2017, he founded the Green Communities Foundation, supporting over 220 housing societies and diverting 4,000 tonnes of waste from landfills through aerobic composting.
In Buragunte, a village tucked into the fringes of Sarjapura, under the quiet insistence of Lalitha Akka, a shift began. What if, she asked, the leftovers didn’t have to vanish into some distant, smoking heap? The women in her village brainstormed. They began to pile their kitchen scraps into small pits behind their homes, and weeks later, they harvested compost that they folded back into the fields.
Meanwhile, in the digital sphere, “Worm Rani” has become an Instagram star. With over 300,000 followers, Vani Murthy’s reels demystify composting and sustainable living. From her terrace workshops to speaking about using reusable steel cups, she models a life where composting is less an eco-chore and more a meaningful daily ritual.
Inspired by Worm Rani, composting warrior Anisha Nayak began her own journey from reluctance to triumph. Her balcony, once a storage space, is now home to a terracotta compost setup—later upgraded to a sleek Khamba unit from Daily Dump. Two years later, not a scrap of green waste leaves her home.
Also read: Setting up a compost bin at home: Do’s and don’ts for feed and airflow
From professional waste management companies like Earth5R, DailyDump, Sampurn(e)rth, RUR Greenlife, My Green Bin, and Green Legion, to municipal programs offering composting kits and collection services, help is everywhere.
If you feel intimidated, start small. Pick a composting method that works for your space. Engage with your community. Share your results. Because you’re not alone. And your bin might just inspire your apartment building, your college, your city.
Also read: The science of scraps: How to get composting right
{{quiz}}

Preservative-laden pickles, artificially-flavoured milk drinks—even seemingly harmless foods can be ultra-processed
For as long as we’ve been cooking, humans have been trying to solve one problem: how to keep food from spoiling. Over centuries, we’ve evolved from drying ingredients under the sun to sealing them in factory-made packets. Somewhere between the simple acts of preservation and the crunch of convenience lies the story of altered food.
Step into almost any Indian kitchen and you’ll see food in motion. Rice being rinsed in cloudy water. Milk coaxed into becoming curd with nothing more than a spoonful of yesterday’s batch. These are almost invisible acts of processing—meant to preserve, to prepare, and to make a staple edible without stripping it of its character. Move a little further along the spectrum, and the transformations deepen. Dosa batter fermenting overnight, butter simmered down to ghee, vegetables sliced and left to dry in the sun. Still recognisably food, but reshaped by time and microbes. Push outward, and you reach artisanal processing—commercial blocks of paneer wrapped in cellophane, flour ground and packaged with minimal modification, jars of pickles made to last a season.
And then, at the far end, a rupture: industrial ultra-processing. This is where food is engineered rather than prepared. Instant noodles compressed into bricks, bread puffed up with emulsifiers, curry pastes and ready-to-eat meals fortified with stabilisers and preservatives. Here, salt, sugar, and fat dominate to override satiety and keep you reaching for more. But this was not always the case.
Consider ghee-making—one of humanity's oldest food preservation techniques. Traditional ghee involves slowly heating butter until the water within it evaporates and milk solids separate. This process concentrates nutrients, creates unique flavour compounds, and produces a stable fat that doesn't need refrigeration. In contrast, the manufacture of commercial ghee may start with cheaper oils. It may also contain additives such as butylated hydroxyanisole (BHA) and butylated hydroxytoluene (BHT), added to improve shelf-life, but better known for their debatable health risks if consumed above conservative limits.
Dosa batter fermentation represents another traditional process. When rice and lentils are soaked, ground, and fermented, naturally occurring bacteria and yeast break down proteins and carbohydrates. This increases nutrient bioavailability, creates beneficial compounds like folate, reduces anti-nutrients, and imbues dosa batter with its characteristic tangy flavour. However, instant dosa mixes skip fermentation entirely. The complex biochemical transformations that occur during natural fermentation—which create beneficial compounds and improve digestibility—are bypassed in favour of speed and shelf stability.

Also read: Bastar’s secret ingredient? The power of preservation
Processed foods start as natural or minimally-processed foods but have a few extra ingredients added—like salt, sugar, or oil. They are usually recognisable versions of the original food and are often used in cooking as part of a meal rather than eaten entirely on their own. For example, frozen peas or store-bought plain yogurt.
On the other hand, ultra-processed food often includes substances not typically found in a home kitchen. Its definition continues to evolve, but the generally agreed-upon understanding of the term is any industrial formulation containing five or more ingredients, including stabilisers and preservatives. The food matrix is broken down, meaning nutrients are less intact compared to the original source. Such foods are designed to be hyper-palatable, long-lasting, and ready-to-eat, but look and taste very different from the raw ingredients they came from. Examples: soda, chips, candy bars, flavoured instant noodles, or fruit juice in tetra packs.
India faces a unique challenge: there is no standard criteria for identifying UPFs using a classification system based on the extent and purpose of industrial processing.
If you slice up a potato at home and fry it as chips, it will be considered processed because you start with a natural food (potato), add ingredients like oil and salt, and cook it. The final product is still clearly derived from the original potato, and you’re only using simple ingredients you would normally have in your kitchen. Store-bought packaged chips, however, are ultra-processed since they contain many additives and go through industrial processing methods.
Here are some quick tips to spot the difference between the two categories:
To apply the rule, start by looking at the Nutrition Facts label and focusing on the % Daily Value (% DV) column, which mentions the percentage of your daily diet that the food would contribute to.

India faces a unique challenge: there is no standard criteria for identifying UPFs using a classification system based on the extent and purpose of industrial processing. This definitional gap has led to inconsistent terminology, with descriptors like “junk foods,” “fast foods,” “ready-to-eat foods,” “instant foods,” “processed foods,” “packaged foods,” and “high-fat-sugar-and-salt (HFSS) foods” all being used interchangeably to denote UPFs.
In 2024, researchers in India decided to address this by turning to a more familiar marketplace: the online grocery store. They scanned the labels of 375 brands—at least three for each item—and confirmed 81 foods (including chips, ready-to-serve beverages, breakfast cereals, namkeens, jams, and peanut butter) to be unmistakably ultra-processed. Even some packaged versions of traditional recipes, sold as convenient shortcuts to home cooking, carried the same markers highlighted in the Food and Agriculture Organization’s (FAO) guide to identifying UPFs. The markers included added flavours and colours (to mask unpleasant tastes, smells, or textures caused by ingredients, processing, or packaging), or enhanced the product to make its sensory qualities (appearance, taste, aroma, or feel) more appealing, or both.
The goal is to recognise the difference between processing that enhances food and processing that engineers it beyond recognition.
Twenty-three categories of UPFs emerged from this analysis, revealing clear preference patterns. Breads, chips, and sugar-sweetened beverages topped the list as the most preferred UPFs, while frozen ready-to-cook foods (like chicken nuggets and frozen kebabs) were least preferred—reflecting Indian taste preferences and eating habits.
Commonly consumed, everyday UPFs that many people don't recognise as being ultra-processed include breakfast staples like commercial bread (even the ‘brown’ varieties), packaged cereals, and instant oats with added flavours. The beverages in this segment encompass packaged fruit juices, flavoured milk, and energy drinks. Convenience items, like packets of ketchup and mayonnaise, and seemingly traditional offerings, too, fall into this category—pickles packed with preservatives, commercial chutneys, and packaged spice mixes with anti-caking agents—demonstrating how UPF ingredients have crept into food preparation.
Also read: Food for thought? How our meals and minds are deeply, delicately connected
Indians are purchasing more and more junk food and the health implications are alarming. The Indian Council of Medical Research (ICMR) estimates that 56.4% of India's total disease burden—measured in financial costs, hospitalisation expenses, and lost productivity due to illness, including sick leave from school and work—is directly linked to the rising consumption of junk food.
This shift represents a cultural transformation. Understanding this spectrum helps make informed decisions. The goal is to recognise the difference between processing that enhances food and processing that engineers it beyond recognition.
A good rule of thumb is to look for foods with short, familiar ingredient lists. Whenever possible, choose items that have been traditionally processed. When convenience is unavoidable, take a moment to read the label and select products that stay closest to their original preparation methods. By understanding the difference between beneficial processing and its industrial counterparts, one can make choices that balance health with ease.
Also read: For Odisha’s Chuktia Bhunjias, preservation by drying is tradition—and sustenance
{{quiz}}

Your body’s capacity to digest protein depends on how much you consume at once and what you pair it with
Editor’s Note: From grocery lists, to fitness priorities, and even healthy snacking, protein is everywhere—but do we truly understand it? In this series, the Good Food Movement breaks down the science behind this vital macronutrient and its value to the human body. It examines how we absorb protein from the food we consume, how this complex molecule has a role to play in processes like immunity, and the price the Earth pays for our growing protein needs.
You’ve mixed your rajma with your rice, measured your servings of fish and milk, and are all set to conquer your protein needs. But somewhere along the line you notice that all this meticulous planning is not resulting in better energy, muscles, or hair. What’s going wrong?
Perhaps it is not your protein intake that’s faltering, but rather your protein absorption. The protein may be entering your body, but is it getting broken down into a form that can be processed and used appropriately?
How do our bodies usually absorb protein? Imagine it to be a knotted ball of yarn. Digestion starts when the stomach releases hydrochloric acid and the enzyme, pepsin. Hydrochloric acid denatures the protein (unfolding its complex three-dimensional structures) —essentially, it untangles the yarn. Pepsin starts the process of breaking protein into polypeptides, i.e. cutting the untangled yarn into manageable chunks.
The body can only process around 20-30g of protein every 3 hours. So, you need to space out your intake to ensure your body can use it.
Polypeptides (long chains of amino acids, which are the building blocks of protein) are then passed onto the pancreas, which is the main centre of protein digestion. Proteases is one of the major protein-digesting enzymes released by the pancreas, and it breaks down polypeptides into tripeptides, dipeptides, and lastly, to individual amino acids. Think of the breakdown of polypeptides as separating the yarn into groups of 2–3 threads, or into individual threads. These journey onwards to the small intestine, which breaks down any remaining tripeptides and dipeptides into individual amino acids. These individual amino acids are then absorbed into the bloodstream. They all report to the liver, from where they are deployed across the body for different functions.
But what happens if some protein does not break down into absorbable amino acids? Well, they continue their journey onto the large intestine. The large intestine does not have the enzymes to break down proteins. Sometimes, they may pass through your body unfettered, but they could also become tempting food for the bacteria of the colon. As the bacteria metabolises protein, it releases certain byproducts (including ammonia, sulphides, and valeric acid) which can contribute to various ailments, from inflammation to DNA damage. So, not only does a lack of absorption cut off our access to protein, it risks becoming an active health risk.
Also read: Is there an ‘ideal’ amount of protein that must be consumed?
Why would our bodies refuse to digest protein? There could be multiple reasons. For one, you could be trying to finish off your protein requirement for the day in one sitting. The body can only process around 20-30g of protein every 3 hours. So, you need to space out your intake to ensure your body can use it. Similarly, certain disorders (like maple syrup urine disease) or medications (like antacids) might interfere with protein absorption.
The trickier issue is that not all protein is equally digestible. Its digestibility differs based on its source as well as processing method. For example, dairy proteins are easier to digest than meats (though both have more than 90% digestibility). Plant proteins tend to be a little harder to digest, at only around 70-90% digestibility. One of the main reasons plant proteins are less digestible is that they are more likely to have anti-nutritional factors—compounds which obstruct digestion in some way. These compounds occur naturally in the plant, typically forming part of its immune system.
The lesson here is not to cut out these foods from your meals, but rather to be mindful of how you incorporate them into your meals.
Cereals like wheat and rice, and vegetables and fruits like potatoes and tomatoes, are examples of plant proteins with common anti-nutritional factors. They have certain chemicals that bond with trypsin, pepsin, and other protein-digesting enzymes and inhibit their functioning.
Tea and coffee share a certain astringency with fruits like grapes and pears, because they all have tannins. Tannins bind with the proteins we eat (especially collagen proteins—the proteins which build up our skin, bones, ligaments and tissues) forming a cluster (a process called aggregation). Binding changes their chemical composition such that digestive enzymes are unable to break them down. Garlics, onions and other alliums contain saponins, which also tend to form complexes with proteins resulting in reduced digestibility.
Nuts and seeds form an interesting case, since their impact on protein digestion is indirect. They contain phytic acid which forms complexes in our bodies. These complexes inhibit the absorption of minerals like zinc and calcium, which are in turn crucial in the synthesis of digestive enzymes. Without adequate enzymes, our absorption of nutrition (protein or otherwise) suffers.
Also read: The science behind bodily protein: What are complete and incomplete sources?
Don’t be alarmed: this doesn’t mean that plant proteins are a less reliable source of nutrition. The way we process proteins in our kitchens can improve how our bodies digest them. Age-old practices of soaking, germinating, heating, and pressure-cooking all increase digestibility of plant proteins by reducing the potency of their anti-nutritional factors. One study from as far back as 1989 found that soaking mung beans improved in vitro protein digestion by 4% in 6 hours and 21% in 18 hours by lowering anti-nutritional factors (phytic acid, saponins, and polyphenols) in the legume seed.
Counterintuitively, a lot of common ways to process meat—mincing, salting, irradiation, ageing—are associated with lower digestibility. These processes tend to oxidise proteins, causing them to form strong bonds with each other (called cross-links), which makes them less susceptible to digestion; effectively, the yarn of wool becomes knotted up and harder to unravel. A 2017 study found that long-term pickling and drying, as well as extended high-temperature cooking, reduced the sensitivity of pork protein to pepsin digestion, and consequently the absorption of its protein content by the body.
Age-old practices of soaking, germinating, heating, and pressure-cooking all increase digestibility of plant proteins by reducing the potency of their anti-nutritional factors.
On the bright side, just like some proteins come with anti-nutritional factors, others are rich in enzymes and contribute to protein digestion. Ginger, pineapple, papaya, and honey all contain different protein-digesting enzymes like bromelain, papain, zingibain.
It’d be a natural reaction to read this article and worry about your morning cup of tea, or the tomatoes you’d been enthusiastically incorporating into your salads. But fret not—there are many ways to ensure that the protein you’re feeding your body is being properly absorbed and processed. For one, you can use workarounds: eating cooked instead of raw tomatoes, soaking nuts and seeds before eating them, or shifting your tea time to three hours after your meal can go a long way. But more importantly, food is not a simple binary. Tea and tomatoes are both great sources of antioxidants—as are several other foods with anti-nutritional factors. The lesson here is not to cut out these foods from your meals, but rather to be mindful of how you incorporate them into your meals.
Our bodies undergo thousands of reactions during the process of digestion which interact with each other in ways that are hard to predict and simplify. Moreover, human biology is varied, and our digestive systems respond differently to the same food. We do not yet have a predictable (or affordable) way of measuring our individual rates of protein absorption, which leaves a lot up to us observing our bodily reactions to foods and adjusting our approaches accordingly. It is nice, in a way, to be engaged in a continuous dialogue with our body, don’t you think?
Also read: Protein’s seen and unseen benefits: How it affects metabolism, muscle repair
{{quiz}}

How one man nurtured 100 edible ecosystems across 300 acres
When Shihab Kunhahammed was 10, he planted his first tree—an act contrary to the sterile sameness of childhood routines—inspired by a nonagenarian grandmother with a green thumb, and a Malayalam film about land and longing. Five years later, when he was still in his teens, he realised that working with soil was his true calling, and that much work lay ahead to fulfill his potential.
Eventually, in 2015, at the age of 28, he’d leave behind a career in engineering to find himself in Hosur, Tamil Nadu, standing on a piece of land ready for something wild and breathing. What followed was less a project and more a patient endeavour: a forest, built leaf by leaf, fruit by fruit.

At first glance, Kunhahammed does not have the ‘look’ of an agricultural revolutionary: soft-spoken, slight, and dressed in a manner typically associated with teachers, he speaks with the deliberate care of someone who has learned not to waste words—or resources. “It wasn’t enough to just grow food,” he says, “I wanted to grow systems—ones that could heal land, feed people, and last.”
Kunhahammed’s journey into rewilding began with a deceptively simple idea: the food forest.
Kunhahammed’s journey into rewilding began with a deceptively simple idea: the food forest. Standing in a single spot, he points out in multiple directions at trees of avocado, soursop, amla, star fruit, and multiple mango variants in his forest. Inspired by indigenous farming and refined through permaculture, it layers trees, shrubs, vines, and roots into a self-sustaining, edible ecosystem. Blending this with the dense planting principles of Japan’s Miyawaki Method, Kunhahammed has helped create over 100 such “dense edible ecosystems” across 300 acres in six Indian states—Tamil Nadu, Kerala, Karnataka, Maharashtra, Telangana and Andhra Pradesh. In total, he has planted over 50,000 trees since 2020. “Mulch makes a difference,” he says, stressing the importance of design, spacing, and layering the ground with “browns”, which are carbon-rich materials that feed the forest from within.
Also read: How Miyawaki forests are reshaping urban landscapes
A food forest is a carefully designed ecosystem that mimics the architecture of a natural forest, but everything in it is edible. Like a wild forest, a food forest has multiple layers: underground tubers, low-growing ground cover, shrubs, climbing vines, and short and tall trees. Even cattle may graze among the trees.
But this isn’t wilderness, and it’s not a backyard garden either. A food forest is a deliberate reimagining of how we grow food in a warming world—one that values diversity, soil health, and longevity over monoculture and yield.
{{marquee}}
Most plants are perennial, returning year after year. And while food forests don’t require vast acreage, they do demand time and care. In the early years, they require heavy mulching and weeding; as trees mature, they need to be pruned to keep fruit accessible.
A food forest is a deliberate reimagining of how we grow food in a warming world—one that values diversity, soil health, and longevity over monoculture and yield.
The goal is not to produce the most food as fast as possible; it's to create a system that supports plants, pollinators, animals, and humans alike, season after season.

Also read: How an Alappuzha coir exporter nurtured a one-acre forest
For Kunhahammed, the trees are just the beginning. His food forests aren’t passive green museums; they are active, evolving landscapes. During year-round camps, children who spend time in the forest walk around pointing out plants with the confidence of junior botanists; even his son can identify the flora. “This is amla, that’s mango, and over there—a coconut tree,” his son says. These kids aren’t memorising facts for an exam. They are growing up with food in its natural form, watching it fall from branches instead of emerging shrink-wrapped from shelves.
There’s something almost monastic about the whole operation. Kunhahammed works with the patience of someone who knows the results may outlive him. “It’s not fast,” he admits. “But it’s resilient.” That distinction matters. In a time when even agriculture has been seduced by metrics like yield per hectare and units sold per season, he is playing a longer game. Apart from fruits, his forests offer shade, shelter pollinators, nourish fungal networks, sequester carbon, and cultivate knowledge.

He tells the story of farmers who once had to sell their land or abandon it, returning to find the soil reborn. They now harvest mangoes, turmeric, lemons, and ginger from a space that had once choked on dust. Through seasonal events like ‘Magnifera’, a mango festival that doubles as a farmer's market that attracts around 300 participants, he’s trying to collapse the gap between grower and consumer.
Held every year in the second week of June, the event features a variety of mango-based dishes and showcases multiple mango varieties. Participants also learn about technical aspects, such as measuring the total soluble solids (TSS) of the fruit and how to cultivate them organically. In the last edition of the festival, over 250 varieties were exhibited.

What’s radical here is not the novelty of the trees but the relationships they foster. There’s a slow collectivism at work: seed-saving circles, WhatsApp groups where someone’s banana glut becomes someone else’s supply, composting stations tended to by neighbours. Kunhahammed has developed a community to help coordinate these local economies, though he prefers to rely on the old networks operated through word of mouth.
That romanticism is deliberate. He’s trying to re-enchant agriculture, to make it seem not like drudgery but craft. And yet, the reality isn’t supportive of agriculture. Heatwaves are intensifying. The rain is erratic. Sometimes, entire saplings wither before they root. And bureaucracy is always a hassle.
In a time when even agriculture has been seduced by metrics like yield per hectare and units sold per season, he is playing a longer game.
Lately, his work has begun to draw attention beyond local communities. International organisations have taken notice, and he has been invited to present his methods at global forums, including the United Nations Convention to Combat Desertification, which took place in Riyadh, Saudi Arabia, in December 2024.
Also read: A man dreamt of a forest. It became a model for the world
Yet, despite the recognition, he remains grounded. He urges those interested in agroforestry to begin slowly by experimenting on weekends, understanding the land’s cycles before committing fully. Without a system of support or sustainability, he warns, the shift can become overwhelming. He has seen too many people burn out after diving in too quickly.
There’s a moment when he plucks a ripe custard apple from a branch, eyes lighting up with the unmistakable pride of someone introducing something they’ve helped bring into the world. That same delight surfaces as he shares the fruit with his young son. In these small gestures, there is a quiet, persistent love.
At a time when ecological collapse feels inevitable and institutional efforts appear stagnant, the forests he nurtures stand as living rebuttals to environmental degradation. In a world that is increasingly on fire, Kunhahammed’s project is neither flashy nor does it promise rescue. But it does offer restoration. And that may be enough for now.
Please try another keyword to match the results
