Rama Ranee
|
February 23, 2026
|
12
min read
Raised by nature: Bonds with farms, forests help children grow holistically
Safe spaces, outlets for creativity and curiosity, and a connection to the Earth—nature can mean many things to kids
Read More

What we eat affects our moods, and our moods affect what we eat. What, then, should we do?
From a bag of chips to a handful of chocolates, calorie-rich junk food has come to the rescue of many a stressed-out individual having a bad day. Food—whether junk, homemade or nostalgic—soothes our anger, anxiety, or sadness. The taste distracts us, and the familiarity comforts us. It allows a sense of calm to take over. What’s not to like?
This familiar behaviour of consuming something as a quick fix for a bad mood is called ‘emotional eating’. If you are an emotional eater, you are in good company: a 2023 study among North Indian adults showed that over 70% of those surveyed engaged in emotional eating.
Interestingly, this eating habit was observed to occur at a higher frequency (~82%) among healthcare professionals in Mysuru in a 2025 study, perhaps linked to the high-stress nature of their roles.
It is a bit unfortunate, really, that these foods we reach out for are energy-dense, sugary, fatty, and largely devoid of nutrients. But there is a hidden logic to this misfortune—both biological and psychological. Eating, something that our body associates with nutrition, releases dopamine—a hormone linked to our brain’s reward centre.
However, modern junk food combines sugars and fats in a way that results in a far more powerful reward than any whole food gives us.
Over a period of time, eating fatty foods and feeling good creates a positive feedback loop. When we are stressed, our brain tends to fall back on habits that it associates with feeling good. “Stress hormones disrupt metabolism, and our body ends up utilising a lot of mental energy. At this time, the mind is looking for reward, and one of the most common things to turn to is sugar and fat-loaded food that uplift your mood due to dopamine release,” explains Bhavisha Sancheti, a nutritionist who teaches clinical nutrition as Assistant Professor at Dr. BMN College of Home Science.
Also read: Antibiotic overuse is turning your gut against you
When we crave junk food, there is an anticipatory release of dopamine in our body, as well as the production of ghrelin, the hunger hormone. When we give in to the craving, a second round of dopamine is released; the habit is reinforced. Psychologically, these incidents are categorised together as memories of eating fatty foods and feeling better.
“Boredom and loneliness create emotional existential voids,” Mumbai-based psychologist Dr Anureet Sethi explains, “that increase junk food intake. These foods serve as a coping mechanism to self-soothe and provide quick relief to anxiety and low moods.”
This forms the foundation of why eating fatty foods feels rewarding. At a deeper level, as we keep eating foods that release high amounts of dopamine, our brain tries to restore balance and reduces the amount of dopamine receptors in our body. With fewer receptors to pick up on dopamine, more dopamine needs to be released to reach the same effect. This built-up tolerance leads to overeating, increasing the risk of obesity. It is exacerbated by the fact that most ultra-processed food also interferes with leptin, the hormone responsible for telling us when to stop eating. This is what makes processed food addictive.
The convenience of packaged food also enables opting for it, especially when one is mentally exhausted, Dr. Sethi explains, “Depression or anxiety can reduce the capacity to look after oneself. This disrupts daily routines, including meal planning and cooking, and leads to a reliance on processed food.”
Our food choices are also products of our overarching relationship with food. Happiness does not necessarily guarantee that people eat healthy; however, calmness does. Positive and calm emotions enable us to think about long-term benefit and resisting temptations rather than getting swept away by excitement.
At some level, most of us are aware that processed foods are not good for us. Awareness just fuels guilt and shame if we continue to participate in the same vicious cycle. Dr. Kersi Chavda, a psychiatrist at Mumbai’s Hinduja Hospital, offers an alternative: “Eating more and more sweets and junk food is not sustainable. Rather, you can eat naturally sweet foods like raisins, melons and other fruits. They will give you the same dopamine, and they are much safer as they are natural.”
Sakina Godhrawala, consultation dietitian and clinical nutritionist, suggests consuming food that will calm down your body, like foods rich in antioxidants. “For example, herbal teas like chamomile provide a significant amount of magnesium and also relax the brain and body.”
Also read: Mess on my plate: India’s students are fixing their college diets
The relationship between food and mental health is a two-way street: just like mood impacts our food choices, food choices impact our mental health. Clinical nutritionist Priyanka Chopra explains, “Depression and other mental health conditions are multifactorial disorders, not caused solely by poor diet. Clinical research highlights the interplay between genetic predisposition, environmental toxins, chronic stress, emotional trauma, and autonomic nervous system dysregulation.”
However, it is a crucial facet of our mental health because processed food contributes to inflammation and an imbalance in neurotransmitters that, among other functions, regulate mood. For example, a low-protein diet could lead to deficiencies in essential amino acids like tryptophan and hinder serotonin production. Serotonin is our “happiness hormone”; any deficiency makes itself felt directly on our mood.
A study published in 2023 linked deficiencies in Vitamin B, omega-3 fatty acids, and magnesium to depression. “The review highlighted that lacking these essential nutrients may increase the risk of depressive symptoms, emphasising the role of nutrition at a biochemical level,” asserted Dr. Anjali Chhabria, a psychiatrist, psychotherapist and author.
Not only does processed food deprive us of nutrients we need; it actively contributes to chronic inflammation, which has been associated with depression. “Pro-inflammatory diets (for example, fast food, fried foods, and sugary snacks) are associated with a 51% higher risk of the mental health disorder. High sugar and refined carb intake cause rapid blood sugar spikes and crashes, leading to mood swings, fatigue, and irritability—symptoms that mimic or exacerbate the disorder,” psychologist Dr. Sethi explains.
Also read: Detox teas: Slim claims, heavy consequences
Our mental health also depends on us being good hosts. Confused? Well, our bodies host trillions of microorganisms—and their populations are most dense in the gut, reaching up to 100 billion cells per millimetre. The gut shares a direct cable with the brain called the Vagus nerve, which allows for quick bidirectional communication between the two.
A poor diet affects the good microbes in our gut, while allowing the bad microbes to flourish. “The bad microbes release toxins that can disturb the communication between gut and brain,” Bhavisha Sancheti explains, “This damages the intricate network of the immune system and reduces the formation of chemicals like serotonin that elevate mood.” Given that the gut is home to over 95% of the serotonin produced in our body, this can be a damning turn of events.
Many clinicians have used this knowledge to counter mental health illnesses by reintroducing good bacteria into the patients’ gut. “Patients with depression often have reduced populations of Bifido species, Lactobacillus species, and Faecalibacterium prausnitzii. Coprococcus species, often involved in dopamine metabolism, are also reduced in numbers,” Priyanka Chopra shares.
Similarly, a 2022 study tried examining the influence of a Mediterranean diet on the depression symptoms of young men, and found significant improvement in their symptoms. A Mediterranean diet is a diet derived from the traditional diet of the countries around the Mediterranean Sea, and postulates a plant-based diet with moderate fish and dairy products, emphasising staying away from processed foods. While mental health outcomes were only tested for the Mediterranean diet specifically, one can extrapolate that regional traditional, balanced diets from across the world could have similar effects.
In fact, a study in Australia over 2 years concluded that eating 8 portions of fruits and vegetables a day gave the same increase in happiness as going from unemployed to employed.
These studies offer fragments of knowledge—but a larger wisdom lies in reshaping our relationship with food. Small measures can go a long way.
Ask yourself why you are eating before you eat anything: is it hunger, boredom, or stress?
Prepare strategies in advance for high-stress events where you are likely to slip up. Try eating slowly, allowing your body to send you signals of satiety. Mindfulness goes a long way in combating emotionally-driven eating. Multiple studies have observed how mindfulness calms the amygdala—the part of the brain linked with emotional responses—and hence helps us regulate our emotions better.
Ultimately, good food and good mental health enable each other. This can be a scary prospect for someone with a poor diet or with mental illnesses. However, it also means you have the opportunity to make your health, both physical and mental, better through good nutrition. This is an uphill battle, yes, but one that can be won with some patience, and a lot of compassion for yourself.
Additional inputs by Durga Sreenivasan
{{quiz}}

A forest floor-like aroma, crumbly texture—compost has ways of signalling its maturity
After months of patient waiting (and the occasional worried peek inside), your compost pile will subtly signal its readiness, but how do you spot it? Ready compost doesn't announce itself with fanfare, but rather whispers its arrival to your senses.
Good compost has an earthy, forest-floor aroma—pleasant and fresh, never sour, ammonia-like, or putrid. If you can still identify last week's tomato or detect old newspaper shreds, your compost needs more time to mature. Visually, your compost has undergone a transformation. The peels, tea leaves, and eggshells have disappeared into anonymity, leaving behind a uniform, dark brown substance that looks suspiciously like expensive store-bought potting soil.
Texture tells the story of proper decomposition. Run your fingers through the finished compost—it should feel soft and crumbly, breaking apart easily in your hands. When you pick up a handful, it should feel cool and moist but not soggy, similar to a wrung-out sponge.
The temperature test provides the final (scientific) confirmation. There are compost thermometers in the market for those keen on precise measurements, but your hands can give you an approximate measure too. Mature compost should be cool (less than 90°F/32°C), unlike active compost which generates heat during decomposition. Active decomposition occurs most rapidly between 90-140°F (32-60°C), so if your pile is still warm in the centre, give it a few more weeks to complete the process.
Also read: Setting up a compost bin at home: Do’s and don’ts for feed and airflow
Place a small handful of moist compost into a sealed zip-lock bag, pressing out the air first. Leave it for three days. When you open the bag, if it smells sour or strongly of ammonia, microorganisms are still working and the compost isn’t ready yet.
Also read: Trouble in your compost bin? Here are solutions for stink, slush and surprise guests
For potted plants, which dominate Indian urban gardening, add an inch of compost twice a year. In garden beds, whether you're working with a bungalow compound or a terrace garden, it is also recommended to add an inch or less of compost each year, since excess compost can cause a build-up of nutrients like phosphorus.
Compost can play two roles in a garden bed, depending on how it’s applied: it can be mixed into the soil as an amendment, or spread over the surface as mulch.
When incorporated into the soil, compost boosts nutrient content, balances pH, and enhances soil texture, drainage, and moisture retention. For healthy soils that could still benefit from some organic matter, it’s best to limit digging or mixing to the upper 4 inches of soil to avoid disturbing soil structure and organisms.
When applied as a mulch, compost forms a surface layer that helps keep weeds at bay, conserves moisture, and moderates soil temperature. The process is simple—just spread a layer of compost over the soil surface. Over time, this mulch will naturally deliver the same improvements as compost worked directly into the soil. Unlike chemical fertilisers that provide an immediate but short-lived boost, compost works patiently, slowly releasing nutrients while improving soil structure.
The monsoon season accelerates decomposition while winter slows it down, creating a natural cycle that mirrors the traditional agricultural calendar.
The quantity varies depending on the soil and site, plant selection, compost quality and availability. Most mature (or ready) composts can be used in various situations without serious concerns about the precise amount. Experienced compost users rarely have enough compost for its multitude of purposes and take care to disperse the black gold equitably among their plants.
The monsoon season accelerates decomposition while winter slows it down, creating a natural cycle that mirrors the traditional agricultural calendar. During the rains, your compost pile becomes a hyperactive ecosystem, breaking down organic matter with the enthusiasm of a street food vendor during lunch hour. The seasonal changes mean you can time your compost harvest for the post-monsoon planting season, when your garden is ready for rejuvenation and your compost is at its peak potency.
For best results, avoid using compost on its own in pots, as it's too rich and can hold too much water. Also, if you’re reusing old potting soil, always mix in some fresh compost to revive it. Sieving compost before use can help remove large chunks or unfinished material. Plants like tomatoes and leafy vegetables benefit especially from compost-enriched soil, but be sure to blend it with regular garden soil to maintain pH balance.
Also read: The science of scraps: How to get composting right
{{quiz}}

Our protein needs are subjective. Culture, age, and health all shape the ‘ideal.’
Editor’s Note: From grocery lists, to fitness priorities, and even healthy snacking, protein is everywhere—but do we truly understand it? In this series, the Good Food Movement breaks down the science behind this vital macronutrient and its value to the human body. It examines how we absorb protein from the food we consume, how this complex molecule has a role to play in processes like immunity, and the price the Earth pays for our growing protein needs.
From food packets to fitness trackers, protein follows us like a silent ghost—a nutritional metric measured, counted, and calibrated down to the last decimal. We’re often told to aim for 0.8 grams per kilogram of body weight, a number that sounds precise, even severe—something we must adhere to.
But where did this figure come from? And can one number truly be the ‘correct’ requirement for everybody, in every part of the world?
The short answer? Not quite.
Where your protein comes from matters just as much as how much you consume.
To trace the origins of global protein guidelines, we must follow the trail of nitrogen.
Why nitrogen? Well, protein is the only macronutrient that contains nitrogen; and measuring nitrogen is much more cost-effective than direct protein testing, which often involves more complex techniques like analysing their amino acid profiles. The logic for nitrogen balance studies, the universal standard for measuring protein needs, is deceptively simple: eat food, and then measure the nitrogen going in (from protein), and the nitrogen coming out (in urine and sweat, among other forms). By observing nitrogen balance at different levels of protein intake, researchers can determine the amount of protein needed to achieve a state of equilibrium to support growth. If more is expelled than is consumed or absorbed, your body will resort to breaking down its own tissue and muscle mass for its protein needs.
Based on this method, global bodies like the World Health Organization and the Food and Agriculture Organization (affiliated with the United Nations) came up with this figure—0.8g of protein per kilogram of body weight per day—a threshold meant to prevent deficiency in most healthy adults.
Where your protein comes from matters just as much as how much you consume.
But nitrogen, like humans, is unpredictable. These studies were conducted in controlled settings on specific kinds of bodies—young, healthy and mostly male, with access to stable diets and temperate weather. The weather matters because people sweat much more in humid and tropical climates than in temperate weather, and sweat contains measurable amounts of nitrogen (mainly from urea and ammonia) which traditional nitrogen balance studies don’t account for.
This illustrates a limitation of studies like these which have historically been conducted on only a specific Western demographic: their estimate of nitrogen entering or exiting the body is limited by their worldview. They don’t reflect the contextual lived realities that differ across cultures and demographics, which also determine access to protein. Factors like age, health, digestion, cultural eating patterns, and physical labour also influence how our bodies process and use protein.
Also read: The science behind bodily protein: What are complete and incomplete sources?
The 0.8g recommendation is meant to be a baseline, not an ideal. It reflects the minimum amount needed to prevent a deficiency, and not necessarily what’s optimal for wellbeing, especially because this baseline does not apply uniformly.
For example, The Indian Council of Medical Research (ICMR) recommends slightly higher protein intakes in recognition that Indian diets—largely plant-based and cereal-heavy—may offer less protein. Plant proteins often lack one or more essential amino acids, meaning the body needs a bit more total protein to meet its needs. For example, rice and wheat are relatively low in lysine (an amino acid essential for muscle repair) so a cereal-heavy diet will require more complete proteins like dairy to compensate.
Based on this, the Council suggests 0.8 to 1g per kg of body weight per day as the baseline recommended daily intake for all adults regardless of gender. They recommend a ‘balanced pattern’ of cereal : legume : milk in a ratio of 3:1:2.5 to ensure a comprehensive amino acid profile, following which 0.8 g per kg per day is sufficient. If one is not maintaining that proportion in their diet, 1 g per kg per day is recommended.
There’s a quiet danger in reducing food to a number: we end up valuing a gram of protein over the quality of the meal it came from.
Other needs vary more dramatically. Older adults often require more to maintain muscle mass. Pregnant and lactating women usually need more for bodily repair and growth. Those with chronic illness or inflammation also have greater needs since their body uses and breaks down protein faster.
Children also require more protein for proper growth. For instance, children between 1–3 years need about 1.2 g per kg per day, while those in the 7–12 year range require 1.0–1.1 g per kg per day—both higher than the amount recommended for adults. These elevated requirements reflect the demands of rapid growth and tissue development.
Interestingly, in its 2020 Recommended Dietary Allowance guidelines, the ICMR states that protein requirements remain constant across physical activity levels, even though the energy requirement rises with activity. This runs counter to the conventional understanding that active individuals or athletes require more protein, a view widely reflected in literature internationally. The Council even cautions that athletes’ needs are not as high as commonly believed.
Also read: Is your body low on protein? Signs and impacts of a deficiency
That ‘protein-packed’ snack may help you hit your daily target, but it comes with a side of mystery ingredients your body didn’t RSVP to. Because no protein source arrives alone—it comes wrapped in fat, fibre, salt, sugar, micronutrients, or additives.
Consider this:
Often, what we call ‘high protein’ is just highly processed.
This matters because protein doesn’t act in isolation. The context of consumption—what else it is eaten with, how it is digested, and how it interacts with gut bacteria—shapes how beneficial it truly is.
Plant proteins like dals or millets may come with fewer grams per serving, but they deliver fibre, slow-digesting carbs, and gut-friendly compounds. When paired smartly—like dal with rice, or idli with sambar—they offer complete amino acid profiles without the baggage of cholesterol or preservatives. Well-prepared animal proteins, too, like grilled fish or boiled eggs, can pack in high-quality protein along with key nutrients such as vitamin B12, zinc, and omega-3s.
It is often the cooking method or processing that adds the unwanted elements like excess salt, preservatives, or unhealthy fats to our food.
There’s a quiet danger in reducing food to a number: we end up valuing a gram of protein over the quality of the meal it came from.
Rather than asking “Am I getting enough protein?”, we may do better to ask, “Is my protein source nourishing me in more ways than one?”
The science of ideal protein needs will continue to evolve. New methods already promise more precise insights than nitrogen balance tracking ever could. But even the best scientific method or a singular number can’t stage a coup with holistic food wisdom that considers the whole plate, and eating habits that vary across time, location, space and access.
Also read: Whey to go: A complete guide to protein
{{quiz}}

A growing demand for nutraceuticals is threatening fish populations and marine food webs
The oceans appear vast and resilient, stretching in endless blue horizons and rich with life. Yet, beneath the surface, a more urgent reality is unfolding. Even as the planet warms and marine ecosystems struggle to keep pace, extraction of resources driven by human demand reaches beyond just seafood–environmental costs of which are slowly, but steadily, rising. The World Bank estimates that nearly 90% of the world’s fish stocks are under stress now, either overfished or close to it.
The global appetite for dietary supplements is rapidly growing. The omega-3 fatty acids market, for one–valued at $2.62 billion in 2023–is projected to reach $4.45 billion by 2030. The demand for omega-3 is projected to increase even more with rising awareness about its health benefits. Consequently, this means that extraction pressures will grow in tandem with demand, as the industry prepares to capitalise on this.
Omega-3 fatty acids are polyunsaturated fats that are extremely important to the human body and health: they help our body grow healthy cell membranes, which further ensures many benefits to our heart, brain, metabolism, and immune system. Research even suggests that omega-3 can help manage cholesterol; they also help lower triglycerides in the body, which are fats that, at high levels, increase the risk of heart disease and stroke. There are three types of omega-3s, of which EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) are especially valued. But unlike many other sources of nutrition required to keep the human machine humming, omega-3 is actually not produced inside the body.

And so, they are called "essential fats”: you need to consume them in some form externally, like from your diet or as supplements. Omega-3 are “good fats” that you can get from your diet if you consume oily fish, other seafoods like oysters and shellfish, seaweed, chia seeds, flaxseeds and walnuts; as supplements, omega-3 is available as fish oil, krill oil, algal oil and flaxseed oil pills.
Also read: The promises -- and perils -- of aquaculture
Omega-3 fatty acids are typically sourced from fatty or ‘oily’ fish such as mackerel, cod, salmon, herring, tuna, and sardines, as well as walnuts, soybean, and flaxseed. Fish continue to be the primary source for omega-3 supplements due to a higher EPA and DHA content–that is, the omega-3 obtained from fish have these two, long-chain fatty acids that prove to be beneficial to health. Fish oil was the only widely-used source until the 2000s, when microalgae-derived omega-3 was officially approved for use in supplements by the FDA (as a GRAS notification, or what is called ‘Generally Recognised as Safe’).
Omega-3 is sold in bottles across the world, often labelled as “3x strength” or “wild fish oil”. While the labels offer an attractive–and to a certain extent, valid–appeal, they fail to represent the bigger picture of this industry, and the processes involved in holding it up. Fish-based oil has always been a major component of the omega-3 supplement industry, followed by algal oil, krill oil, and other plant-based sources. While fishing pressure, concern over declining fish stocks, and a demand for vegetarian and vegan options may have pushed for non-fish sources, as of 2023, 83.5% of the total revenue brought in by the omega-3 industry still came in from marine sources, like fish and krill, and in small parts, microalgae.
While the labels offer an attractive–and to a certain extent, valid–appeal, they fail to represent the bigger picture of this industry, and the processes involved in holding it up.

However, while fish oil is the most common source of omega-3, it may not be the best. Fish oil can often be contaminated with heavy metals, pesticides, and other toxic compounds, which are usually fat-soluble; the contaminants dissolve and remain in the oils that are later extracted from fish. Anthropogenic activities–that include industrial and agricultural runoff into the ocean–have introduced these harmful pollutants into the marine ecosystem; they are quickly absorbed and assimilated by fish over time.
In 2008, another source was officially approved for omega-3 fatty acids—the Antarctic krill, which are tiny crustaceans that form the foundation of the Southern Ocean food web. Penguins, whales, seals, and seabirds rely on krill, which are currently being extracted at alarming rates for the fisheries as well as nutraceutical industries.

The Commission for the Conservation of Antarctic Marine Living Resources (CCAMLR), responsible for fisheries management and conservation of the marine ecosystem in the Antarctic, had proposed a management framework. But this framework, which prevented the overharvesting of krill and placed scientifically-backed fishing limits in several areas, expired in 2024, mainly because the CCAMLR could not, in time, finalise a revised management plan before the expiration date. With no consensus on a new framework in sight, catches of Antarctic krill are expected to increase beyond what the ecosystem can sustain, at a rate faster than the krill populations could realistically recover at.
The spawning and reproduction of Antarctic krill are dependent on the climate, seasonal sea ice conditions, and oceanic currents, all of which are now affected by climate change, further impacting their numbers. The Antarctic krill fishery is the largest fishery by weight in the Southern Ocean, and most of the fishery extracts are concentrated in regions where marine animals are known to feed on them–essentially depleting natural feeding grounds.
Also read: The perilous future of Kashmir's once-abundant trout
Interestingly, humans are not the only ones relying on fish and krill. Krill fisheries not only cater to the omega-3 supplement industry, but also aquaculture and unusually, the pet cat and dog food industry. Nutrients extracted from krill, including omega-3 fatty acids, proteins and antioxidants are key constituents of pet food. Similarly, large-scale aquaculture relies heavily on fish feed and oil, extracting large amounts of the natural food from the oceans to channel into aquaculture.
Krill fisheries not only cater to the omega-3 supplement industry, but also aquaculture and unusually, the pet cat and dog food industry.
Some of the fish commonly sought for omega-3 fatty acids—sardines, anchovies, herring, and mackerel—are also ‘forage fish’. These are small to medium sized, highly productive pelagic (open ocean) fish, and along with krill, they form a critical and large resource that most marine animals subsist on in food webs. Krill and forage fish are crucial prey for several other larger fish species; they are considered a ‘keystone species’ for their important role in the food chain. Removing them at industrial scales is not just reducing biomass, it is reshaping entire ecosystems.

Forage fish are attractive for fishers seeking short-term commercial gains due to their aggregating nature which makes them easy to catch. They make up around 30% of the global fish catch, a large proportion of which is now being used in aquaculture. Antarctic krill too, are relatively low-effort catch due to the large aggregations they are found in. In 2024, the Antarctic krill fishery closed early after record catches sparked concerns about overharvest and the impacts on the wildlife that subsists on krill.
Asia-Pacific is projected to be the fastest growing market for omega-3 supplements, with highly populated, fast-growing economies like India and China leading the way. While fisheries are fairly regulated globally, there is limited or poor enforcement in some pockets, which could be a cause for concern in the long term.
All of this extraction is happening against the backdrop of climate change, which is already straining the ecosystem. Overfishing and the resultant loss of biodiversity can make oceans less resilient to the vagaries of climate change. Precautionary approaches, ecosystem-based management, and international cooperation with mutually-agreed caps to keep extraction within sustainable limits might work, but it remains to be seen.
Also read: The intertwined fate of Navi Mumbai's Kolis and the Kasardi river
Omega-3 is important, and it makes up nearly 25% of the total fatty acids found in the brain’s grey matter. So, if not krill- or fish-derived oil, what is the alternative?
The good news is that alternatives are emerging, and some have existed for a while. Algal oil, derived from marine microalgae, can replace fish- and krill-derived omega-3s, delivering the same EPA and DHA without impacting marine food webs. These microalgae are phytoplankton—tiny, microscopic plants that fish feed on—and the source of fatty acids for fish. Marine algae-based extraction will reduce dependence on fish and krill, offering a more sustainable source for an important supplement. Algal oil has also been found to be cleaner, richer, and devoid of the odour and heavy metal contaminants often found in fish oil.

While marine microalgae-based omega-3 fatty acid supplements are unlikely to replace fish- and krill-derived oil completely, the data does indicate a shifting trend that could restore some balance.
While there are several logistical constraints that prevent industries from scaling up algae production and algal oil extraction, there exist innovative techniques that ensure high-quality extraction without the worrying environmental impact. The algal oil-based omega-3 market is undergoing a shift, and ‘sustainability’, ‘plant-based’, and ‘traceability’ are the buzzwords driving this revolution. Valued currently at $1.6 billion, it is projected to grow to $2.68 billion by 2030, pushed by consumer preference for alternatives.
While marine microalgae-based omega-3 fatty acid supplements are unlikely to replace fish- and krill-derived oil completely, the data does indicate a shifting trend that could restore some balance. Furthermore, emerging research shows that even some macroalgae or seaweeds can offer similar omega-3 benefits, albeit on a smaller scale. Improved innovation, increased consumer awareness, and consumers making informed choices, could well change the dietary supplement landscape in the years to come.
{{quiz}}

Being mindful of the presence of wild animals can help conserve agrobiodiversity and reduce crop loss
Editor’s note: To know Rama Ranee is to learn about the power of regenerative practices. The yoga therapist, author and biodynamic farmer spent three decades restoring land in Karnataka, envisioning it as a forest farm in harmony with nature. In ‘The Anemane Dispatch’, a monthly column, she shares tales from the fields, reflections on the realities of farming in an unusual terrain, and stories about local ecology gathered through observation, bird watching—and being.
On a boulder to the north of the Bannerghatta National Park, facing the Suvarnamukhi Hills, lies the Anemane Farm. A tarred road, once an old dirt track, snakes down from our village Kasaraguppe to the national park 4 km away, and Bengaluru city thence. Bamboo thickets cover much of the hill sides. Taloora Lac trees (Shorea roxburgii, or ‘Jalari’ in Kannada) rear their evergreen crowns among bare rocks.
The farm shares the national park’s topography and natural vegetation; the average elevation is about 900 m, the GPS coordinates being latitude = 12°48'45.85" N, and longitude = 77°34'02.73". Among India’s largest scrub forests, Bannerghatta serves as a vital link between the Eastern and Western Ghats, and is critical for the conservation of many threatened large mammals. The assigning of national park status has facilitated the restoration of green cover, and consequently, a resurgence of wildlife since the 1970s.

Significantly, it is one of the oldest habitats for the Asian elephant (Elephas maximus).
We are privileged to share this unique landscape with elephants and other wildlife. However, their impact on land use and farmers’ livelihoods is immense. Over the years, a benign acceptance of elephant presence near human habitations has changed potentially into conflict, chiefly due to damage to crops and threat to human lives.
Significantly, it is one of the oldest habitats for the Asian elephant (Elephas maximus).
The causes are complex, and beyond the likes of us to discern. As farmers, our concerns are immediate and practical: it is difficult to predict what the next herd or individual may or may not do or eat. Every season is an experiment and an adventure. It has taken 30 years and a fair measure of resources to arrive at a list of ‘safe-crops’ and some realistic expectations.

This is how a typical morning at Anemane unfolds: The mist lifts, unveiling fields of citrus. I wait for the sun’s rays to reveal paths, not wanting to step into the unknown. Elephants are amorphous, melting into the vegetation. There are a couple of young tree branches on the ground and heaps of ripe figs on fresh elephant dung. The old Cluster Fig tree has withstood such elephant forays and is none the worse for it. As for the rest of the farm, it has undergone waves of transformation with emerging patterns of elephant activities and behaviour.
Like other communities at the forest’s edge, Kasaraguppe, too, has its share of encounters with these animals and continues to grapple with them. I wondered how farmers in the past managed to put down their roots, raise crops and families. An old-timer whose services we fortunately enjoy opened a window to those bygone times: Rajappa’s was one among eight families which migrated from Tamil Nadu in the late 1950s, in search of greener pastures. The land, as it turned out, was a hilly wilderness. Bamboo thickets were cleared and terraces wrought from slopes for fields of ragi, groundnut, flowers and paddy in the valleys. There were grasslands for livestock on the hills. As time turned under the yeoman’s plough, there was contentment—though leopards posed a threat to domestic animals, and wild pigs restricted their choice of crops.
Also read: At Ammachi’s farm, the impossible can be achieved—and made profitable
In 1971, the Bannerghatta National Park was inaugurated. This event was associated with the arrival of elephants to Kasaraguppe by the farmers. Initially, it was a rare occurrence; an occasional herd would pass through, peacefully. Once Chikka Bodappa, one of Rajappa’s fellow villagers, planted ragi with great care. That year, an elephant strayed into his field and tasted a small clump of the millet. Bodappa’s yield was ten times above the normal amount, which he attributed to the blessings of the visitor. Its pad mark was worshipped with reverence, and the villagers treated to a festive lunch. This set the trend for other farmers who began to invoke the blessings of the ‘sacred’ elephant in the hope of bountiful harvests. Rajappa ruefully admitted that there was not a single household that escaped the magical spell of the myth—and Chikka Bodappa’s good farming methods were disregarded in the process.
As the pad imprints in fields multiplied, the farmers despaired and sought respite from elephants.
As the pad imprints in fields multiplied, the farmers despaired and sought respite from elephants. The ragi and paddy seasons required utmost vigil, and the families banded together, braving rain and shine to fend the animals off, sleeping in the fields for days. There was a growing urge to give up farming. Such was the scenario when we began to farm.

Also read: A man dreamt of a forest. It became a model for the world
The ten-acre land in our possession was degraded: bald rocks dotted an undulating terrain, pockmarked with shallow granite quarries. Fallow fields baked under the sun, bleached from generous inputs of chemical fertiliser with a sprinkling of granite dust. The soil was shallow and varied in depth, susceptible to erosion. The Cluster Fig in the valley was a lone sentinel over an elder’s grave. Rain brought to life streams; a swift little one gurgled along the edge of our land, and muddy cascades turned the valley into a marsh, often washing the fields away.
Restoring soil fertility became our primary goal. Defunct quarries turned into ponds to harvest runoff from the hill. Seedlings of local varieties such as the Pongam tree (Pongamia glabra, or ‘Honge mara’ in Kannada) were raised and planted along the periphery to arrest erosion and build up organic matter. Teak and silver oak in the interspaces of fields served as wind breaks. The edges bordering the forest were left alone for native species to revive.
Efforts at regenerating the land were rewarding, but with them came unforeseen consequences: our ponds served as watering holes, and the wooded valley— sheltered by bamboo and the wilderness bordering the forest—was virtually an elephant ‘camp’.

Manure infused life into the depleted soil, sustaining guava, papaya, lemons, and pomegranates, while contributing a new crop of trees, Maha-neem (Melia dubia, or ‘Kaadu Bevu’ in Kannada). The papayas were a sweet success but only briefly; the first time an elephant herd stomped into the fields, all the papaya stems were snapped. None were eaten. After the occurrence of similar episodes, we realised that elephants destroy fine stemmed trees like Moringa and Hummingbird (Sesbania grandiflora, or ‘Agase Mara’ in Kannada).
Efforts at regenerating the land were rewarding, but with them came unforeseen consequences: our ponds served as watering holes, and the wooded valley— sheltered by bamboo and the wilderness bordering the forest—was virtually an elephant ‘camp’.
The saga of a fruit farmer’s unfulfilled dreams further unfolded with a special variety of banana, Nanjangud rasabale. They never saw the light of the day! An elephant in a banana field is like a kid in a candy store. It was of little consequence that the entire village had gathered to chase them away.
Coconut palms met a similar fate. The first flush of flowers caught the elephants’ superior olfactory sense. It was a carnage: within a year, a hundred palms were mere shells left to wither away. When Ratnagiri alphonso mangoes began to fruit, every elephant that passed by helped itself to not just the fruits, but also the branches—possibly to rub itchy backs or merely on a whim. Along with the mangoes went guavas and sapotas, too. After 20 years of trying to revive the stunted, damaged trees, we finally cut them down to prevent further raids.

An elephant’s playfulness is further incited by water bodies and slush. Our paddy field has been akin to a playground. One utterly dark, rainy night, the silence was shattered by deep groans and roars; the earth trembled beneath our feet, literally. The next morning, we saw that the erstwhile paddy field had turned into pools of sludge and mush. The banks had all but disappeared. The only evidence of the night’s revelry attributable to elephants was the scoured floor and imprints of bodies.
Elephants are vigorous post-monsoon, when paddy and ragi ripen. With some luck and nightly vigils, many households managed a harvest, prompting us to sow seeds for several years. Our hopes were raised periodically by the forest department’s assurances of elephant-proofing with solar fencing, trenches, and massive rubble walls. At best, these offered a short reprieve.
Once the other farmers gave up, it became difficult to sustain these crops. Our final attempt was a small patch of paddy grown according to the System of Rice Intensification (SRI) which would have led to a bountiful yield had a lone elephant bypassed the field. We retrieved some of the stalks and piled them up in a rick for the cows. A few days later, the rick was a messy heap—the paddy straw pulled out and consumed, while the sorghum was left uneaten. The lone elephant had discovered the way from the paddy field via the lemons to the rick; not much of a distance, but until then, it was an untrodden path.
Paddy, ragi and fruit farming seemed fraught with risks, so we directed our efforts to millets, legumes, vegetables, flowers, and varieties of citrus. For four blissful years, the fields hummed with bees. Gourds, tomatoes, cucumbers, ladies’ fingers, marigolds, and chrysanthemums thrived, until an elephant acquired a taste for sorghum and avarekai (hyacinth beans), and seemingly memorised our planting calendar as well. Winter and early summer vegetables, crucifers, gourds and tomatoes were sought after. There were many styles of operation, not necessarily a rampage. To explore the contents of a covered patch, a particular tusker punctured the net neatly and then barged in to feast on cabbages.
Also read: No monkeying around on this kiwi farm
Our options have been whittled down to citrus, spices, aromatic herbs, medicinal plants and flowers. Yet, the success of ashwagandha, with immense healing properties and importance in Ayurveda, was short-lived. Just as they were fruiting, the plants were neatly uprooted, and mature roots—the most valued part—eaten.
Nutritional needs otherwise accessible in a natural environment are supplemented through successful forays into farms. Elephants mark territories for specific crops and establish pathways though farmland and forest.

Variations in foraging behaviour—dietary preferences, if one may call them that; the number of individuals; the composition of the herd in terms of age and gender, from stealthy, lone night raiders at touching distance, to a club of boisterous young bulls are all factors which determine the extent of damage. Recently, we were the target of three young bulls who met at the edge of our farm and branched out towards preferred dining. One of them had a penchant for our tamarinds. Such behaviour is not only risky, but I expect, problematic, too, with associated health risks, as it disrupts the elephants’ normal habits of foraging in the wilderness.
Elephants are a part of the agricultural landscape on forest edges, enriching the soil with their dung, eliminating certain plants, while introducing some through seed dispersal, thus contributing to the diversity.
Three decades of appraisal has yielded the finalists which have stood the test of time and might even fulfill their life cycle. Among the cultivated plants, citruses are the front runners. Native trees such as Maha-neem, Taloora Lac, and Flame of the Forest (Butea monosperma), varieties of Terminalia (such as Arjuna, Crocodile Bark Tree, Black Myrobalan and Belleric Myrobalan), bamboo, shrubs including wild edibles, have flourished unbridled and untouched by elephant activity, turning the land into a green haven.

If farming is all about market success, then we are utter failures. The choices we made, some by intent and a few out of ignorance, have determined the outcomes. The prism of success, in economic terms, offers a narrow perspective. In the real sense, regenerative farming ensures long term food security. It contributes towards support systems that enable life. Restoration of soil fertility and conservation of agrobiodiversity through ecologically sensitive farming, integrating holistic practices, have been our chief concern. In that respect we have evolved, if the diversity of birdlife—more than 145 species in an area of 0.05 sq km—is any indication.
Elephants are a part of the agricultural landscape on forest edges, enriching the soil with their dung, eliminating certain plants, while introducing some through seed dispersal, thus contributing to the diversity. For instance, Wild Guava (Careya arborea, or ‘Goujal Mara’ in Kannada), a favoured elephant food that is disbursed by them, is well known to local folk health traditions. Recent studies explore its medicinal potential.
Being mindful of elephant presence and foraging behaviour can help farmers make better choices in terms of crops and planting cycles, thereby reducing losses while conserving agrobiodiversity—the key to sustainability. We are witnessing an increasing fragmentation of wild spaces and forests. Sharing a border with a forest makes us even more aware of our role as a stepping stone and a habitat for a host of organisms, big and small. A forest farm committed to ecologically sensitive farming can serve a vital function.
{{quiz}}
Artwork by Khyati K

Most of our waste ends up in landfills, which pose risks to public health and the climate
Editor's Note: In this series, the Good Food Movement explores composting—a climate-friendly, organic way to deal with waste. We answer questions about what you can compost, how to build composting bins and how this process can reshape our relationship with nature and our urban ecosystem.
If you’ve ever walked past a roadside garbage dump, you are familiar with the exact odour that overwhelms your sense of smell: a blend of rotten eggs, urine, and metal. You may scrunch up your face, pinch your nose, and hurry past on tiptoe, but it will be to no avail. The smell spares no one.
If a small roadside garbage dump creates such an effect, a designated landfill is only worse. The smell is potent enough to sting your eyes, soak through your clothes, and stick to your skin long after you leave it behind. And what you can’t smell, seeps into your veins: methane and carbon dioxide – odourless gases notorious for their role as greenhouse gases, which also restrict the body’s access to oxygen.
For many of us, walking away from the horridness of a landfill is easy. But thousands of people are subjected to this biohazard everyday—they collect, transport and manually scavenge this waste with little to no protection. As long as waste is indiscriminately generated in urban India, landfills will continue to pile up, and manual scavenging—which has deep roots in caste—will continue to be a reality.
Most international guidelines require at least a 500 m buffer zone around all landfills, and the Karnataka state government goes so far as to require a 1 km buffer zone around all landfills. By the government’s own admission, most buffer zones are encroached given the scale of overpopulation in most cities.
Every day, the Bengaluru Urban district generates 4593 tonnes of waste, of which 2399 tonnes (52%) is food waste. In reality, the amount of food waste is likely higher—these figures indicate the separated wet waste that made it to urban collection centres. The municipal corporation operates separate dry and wet waste processing centres. In certain areas, waste is composted or recycled before sending unreusable waste to landfills—for instance, out of the separated 2399 tonnes of food waste, only about 55% (1328 tonnes) gets converted to compost. At other centres, all waste is sent directly to landfills without processing.
Most gases in landfills come from anaerobic decomposition of organic matter—and over 45-60% of landfill gas is made up of the greenhouse gases mentioned earlier: carbon dioxide and methane. Though chemical waste like discarded metal, cosmetics and toiletries can still create toxic compounds like benzene, reducing organic waste in landfills is a sure shot way of reducing not only greenhouse gas emissions, but also the production of foul-smelling gases like hydrogen sulphide.
Bengaluru’s city municipal corporation, the Bruhat Bengaluru Mahanagara Palike (BBMP) has earmarked Rs. 1,400 crore for Bengaluru Solid Waste Management Limited (BSWML) for 2025-26. Of this 1,400 crores, it expects Rs. 750 crore to come from a newly implemented user fee for waste collection. This user fee has invited skepticism from both the public and the media, who disparagingly refer to it as 'garbage tax.' It ranges from Rs. 10 to Rs. 400 per month, and has been incorporated as a component of property tax since April 2025. BSWML currently spends around 590 crores per year on the collection and transportation of municipal solid waste. In a tender dated June 2025, it estimated the costs of secondary collection and transportation (i.e. transporting waste from processing centres to landfills) to be Rs 1,590 crore.
Let's be clear: this money is being used to drive our waste about 40 km every day—using fuel and blocking traffic only to end up in a landfill. Waste put in landfills does not go anywhere; rather, it becomes our heritage. Aptly called 'legacy waste', its informally agreed upon definition is waste that has languished in a landfill for more than a year. Formally, it remains undefined by any Indian authority.
Generally, urban local bodies are recommended to employ biomethanation when they are processing more than 50 tonnes per day (TPD) since it is only cost effective at scale. At a small scale, composting is championed because of minimal technology and investment requirements.
Not only does the waste in landfills take up valuable space, it damages the surrounding environment. It produces leachate, which is a contaminant formed when water flows through the waste, and results in groundwater contamination. Though modern landfills are lined with impervious materials like (ironically) plastic, some amount of seepage or leakage is inevitable in any landfill over a period of time.
As a Karnataka High Court judgement aptly states: 'Landfills are only temporary solutions and long term measures have to be initiated by all concerned authorities as a permanent solution.'
Landfills are also a health hazard to everyone living in their vicinity. In addition to damaging respiratory health, they also contaminate groundwater, crops, and even milk. Most international guidelines require at least a 500 m buffer zone around all landfills, and the Karnataka state government goes so far as to require a 1 km buffer zone around all landfills. By the government’s own admission, most buffer zones are encroached given the scale of overpopulation in most cities.
Also read: The circular bioeconomy movement can change how we see waste
If landfills are not a permanent solution, what is? In the Indian context, an effective approach that stands out is the circular economy. A circular economy is a system where instead of completing a linear life cycle and ending up as waste, materials keep getting circulated through processes like maintenance, recycling, or refurbishment. The subset of this philosophy that applies to bio-resources is called circular bio-economy, and deals with repurposing bio-materials.
Two fundamental pillars of the circular bio-economy are composting and biomethanation (the process of converting organic matter to biogas). Generally, urban local bodies are recommended to employ biomethanation when they are processing more than 50 tonnes per day (TPD) since it is only cost effective at scale. At a small scale, composting is championed because of minimal technology and investment requirements.
Eighty percent of Alappuzha households now have either biogas plants or pipe composting systems; the rest have their waste collected and sent to a municipal composting unit.
Currently, most of India's local bodies process some portion of their wet waste into compost or biogas, either outsourced or through municipal composters and biogas plants. Collectively the waste processed amounts to roughly 49.5% of the total wet waste collected nationally. But these figures vary widely internally across municipal bodies, and still involve transportation costs to municipal composting centres.
It is far more efficient to decentralise the process and set up small local composting units in individual houses or housing societies. The compost it yields can be used by resident gardeners and green spaces within housing societies. Excess compost can be sold to farmers or even nearby nurseries and serve as an additional source of income.
Also read: Don't dump it, compost it: Why peels and scraps shouldn't be tossed into your garden
However, this doesn’t mean that the onus of responsible waste management should shift from the state to the individual. Individual efforts can lay the bricks of change, but administrative support must bolster it. Some Indian cities have made phenomenal changes to their waste management system. The most notable of them is Alappuzha, Kerala, which was recognised by the United Nations Environment Programme (UNEP) as one of the world’s five most pioneering cities with respect to solid waste management.
The story of Alappuzha's transformation started with the people living next to the landfill refusing to allow waste disposal in their neighbourhood. After multiple failed negotiations, the municipality came up with a fresh framework for segregation and disposal. Eighty percent of Alappuzha households now have either biogas plants or pipe composting systems; the rest have their waste collected and sent to a municipal composting unit.
Similarly, the Indian Institute of Human Settlements (IIHS) launched a City-Farmer Partnership for Solid Waste Management in Chickballapur in Karnataka. Under this initiative, wet waste is collected from the municipal council, transferred to compost pits at farmlands, turned into compost, and given to farmers for free. Within just 6 months, over 109 farmers received 759 tonnes of compost.
Composting dominates conversations around soil rejuvenation, and rightfully so. But it has a paired benefit: reducing the strain on our solid waste management system. The circular bioeconomy flourishes when backed by administrative bodies that are deeply invested in equitable and sustainable civic care for its citizens. We must urge our governments to mobilise around the circular economy. And while we wait for policy to take shape, we must take ownership of the waste we generate. Composting is one of the simplest and most accessible ways to get our hands dirty, and change the fate of what would go into landfills to create something that fuels the land instead.
Also read: Trouble in your compost bin? Here are solutions for stink, slush and surprise guests
{{quiz}}

Smelly, potent, and packed with nutrients—chicken poop fuels farms.
Chickens—we know them, we love them, and probably have been chased by one down a lane at least once in our lives. They peck, they cluck, they run around like tiny, feathery dinosaurs who popped right out of Cher’s closet. And…they poop, a lot, like once in every 20-30 minutes.
The average chicken produces approximately one cubic foot of manure every six months, which is equivalent to almost 30 litres of manure—a small suitcase full of poop. And some people have dozens of chickens, so imagine waking up every morning, opening your back door, and being greeted by a mountain of freshly made, steaming-hot (potential) fertiliser.
Chicken manure stands out because it delivers a balanced nutritional profile. Unlike other fertilisers that comprise the primary trio of nitrogen, phosphorus, and potassium, chicken manure naturally contains a larger number of essential nutrients that plants require for optimal growth, including critical micronutrients like calcium, magnesium, sulfur, iron, manganese, zinc, copper, and boron, that are often overlooked but vital for plant health.
Chicken poop is rich in nutrients because chickens eat a mixed diet, and their bodies pack those nutrients into a form that plants can easily use. The organic matter in chicken manure also improves soil structure and water retention while feeding beneficial microorganisms, creating a living soil ecosystem rather than just delivering a quick nutrient fix.
In Bhopal, a (2004) study found that combining 75% NPK (a fertiliser labelling convention pointing to the presence of nitrogen, phosphorus, and potassium) with poultry manure produced better yields than with farmyard manure, a variant made of manure from various farm animals like cows and sheep, mixed with bedding materials like straw, especially for sorghum.
For a farmer, chicken poop is gold. However, one can’t just go around spraying and dumping raw manure onto their plants. It is something like a nuclear reactor; if not handled properly, it’ll straight-up burn everything in sight because of the nitrogen and ammonia present in it. Imagine what your body might go through if one evening you decided to replace your nerve-calming, 100% caffeine-free chamomile tea with a dozen shots of espresso.
That’s why the droppings need to first be composted for them to break down and mellow out. The process is also necessary to eliminate all the nasty little pathogens that could ruin the crops. If done right, what was once a pile of steaming horror turns into plant food. Farmers must also be mindful of which crops they use the manure on. For example, root crops that have direct contact with the soil—such as potatoes, carrots and beets—are a no-no because of the risk posed by pathogens within the manure. They can remain in the soil for weeks and possibly contaminate crops.
Composting chicken poop comes with its challenges. First, the overpowering smell of filth. If you’ve ever had the pleasure of being downwind of a fresh pile of chicken manure, you know what we mean. A poorly managed pile of chicken poop smells like someone bottled all the obnoxious odours under the sun and then shook it up for fun. That’s why experts suggest you keep the pile well-aerated, because nothing ruins neighbourly relations faster than an unexpected wave of Eau de Chicken Butt drifting across the kitchen window.
There’s also the pathogen problem. Raw chicken poop can carry notorious bacteria like the infamous E. coli, Salmonella, and a bunch of other microscopic nightmares. Being careful while handling it is crucial. So, wear gloves, wash your hands, and let the droppings cure for 45-60 days before. Also, add carbon-based materials like leaves, straw, wood shavings, or wood chips to balance the nitrogen in the manure and dial down the odour.
If you don’t have access to fresh chicken poop or don’t have the time to process it yourself, worry not, because that concern has already been taken care of by the agricultural experts. One can actually buy dried, pelletised chicken manure in bags across the internet.

Also read: Meet the minds investigating bugs lurking in poultry
Farmers have been using chicken manure for centuries. There’s even archaeological evidence that the first domestic chickens appeared around the time humans began cultivating rice and millets. Basically, ancient humans saw jungle fowls hanging around their crops and thought, “Let’s invite them over.” Ever since, the little feathered freeloaders continue to repay the favour the only way they know how—by pooping.
In Tamil Nadu, particularly in Namakkal and Erode, poultry manure is widely used in millet cultivation. Farmers also sell this manure to neighbouring states, where it is applied to vegetable farms, rubber plantations, and coconut orchards. A study involving 62 poultry farmers in Assam and Karnataka found that nearly 90% of them reused poultry waste as manure on nearby fields. In Nagaland, backyard poultry manure is incorporated into organic farming on a small scale, either through composting or direct application by smallholder farmers, with no involvement from large commercial operations. Additionally, research conducted at the Agricultural Research Farm at Banaras Hindu University in Varanasi demonstrated that poultry manure used in maize cropping systems led to improved yields and enhanced nutrient uptake.
Chicken manure stands out because it delivers a balanced nutritional profile.
In Bhopal, a (2004) study found that combining 75% NPK (a fertiliser labelling convention pointing to the presence of nitrogen, phosphorus, and potassium) with poultry manure produced better yields than with farmyard manure, a variant made of manure from various farm animals like cows and sheep, mixed with bedding materials like straw, especially for sorghum. In Pune, baby corn trials (in 2009) showed that poultry manure led to the highest nutrient uptake and cob yield.
Globally, chicken manure has shown superior performance. A forage crop study found poultry manure boosted fresh yield by 145% and had roughly three times the nutrient content of cow manure. Very recently, in New Zealand, 20-25% higher yields were reported for maize and other crops, compared to cow, sheep, and pig manure. While cow manure improves soil structure, poultry manure offers more concentrated nutrients.
India currently does not provide direct subsidies exclusively for chicken manure. However, several states, like Goa, Bihar, Uttar Pradesh, Haryana, Tamil Nadu and Nagaland, financially support poultry farm establishment (which produces manure).
If you have chickens and are planning to use the manure, you’ll also have an endless stream of chicken poop mysteries to solve. A lot about a chicken's health is revealed just by looking at its droppings. Too watery? Excess protein. Green and foamy? Possibly a disease. The moment you start raising chickens, you become a professional poop detective on the coop scene.
Whether you’re a farmer, a gardener, or just someone who loves a good omelette, somewhere, a chicken and its poop are working overtime behind the scenes, making sure we all stay fed.
Also read: Black Soldier Fly: A hero of insect farming and waste management
{{quiz}}
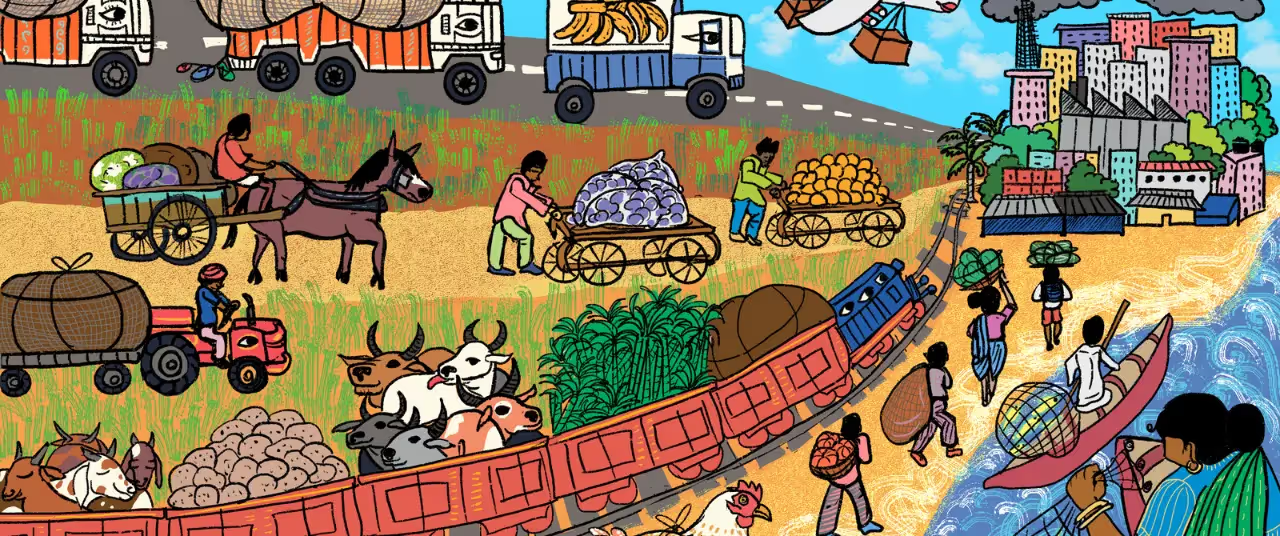
Behind well-fed metropolises are street vendors, produce that travels many kilometres, and fragmented supply chains
The Plate and the Planet is a monthly column by Dr. Madhura Rao, a food systems researcher and science communicator, exploring the connection between the food on our plates and the future of our planet.
Every morning, as India’s cities slowly come to life, crates of vegetables and fruits—some harvested just hours earlier in fields nearby—are unloaded in wholesale as well as Agricultural Produce Market Committee APMC (APMC) markets. Street vendors ready their carts for the day’s trade, small eateries fire up their stoves to serve the first wave of officegoers, and shelves at local grocery stores and supermarkets are stocked in preparation for the day ahead. Day after day, this quiet choreography sustains the vast and often invisible system that keeps cities fed.
But as India’s metropolises expand, these well-rehearsed routines are being reshaped. In this column, I take a closer look at what it means to feed a city fairly and sustainably in such a changing landscape.
Across the country, food reaches urban centres through networks that span vast and varied geographies. These supply chains link remote farms, peri-urban fields, fisheries, livestock holdings, and processing units to urban markets, grocers, eateries, and homes. Food in India travels shorter distances on average, compared to large industrial countries like the US. Food reaching American cities travels over 1,600 km per metric tonne; at around 480 km per metric tonne, food supply to Indian cities averages less than a third of that, owing to more regionally embedded production systems.
Chennai offers an insightful example. In 2020, as COVID-19 lockdowns disrupted lives and economies, the city’s food system came under sudden strain. The closure of Koyambedu market, one of Asia’s largest wholesale hubs and a vital artery for fresh produce, raised urgent questions: how does a metropolis like Chennai get its food?
The Urban Design Collective’s project, Who Feeds Chennai? emerged in response. The initiative traced the movement of vegetables, among other staples, and found that the city’s fresh produce was largely sourced from its peripheries as well as adjoining districts. Another study conducted by IIT Madras found that traders based in Koyambedu, many of whom are unionised, handle the logistics of transport. Smaller farmers unaffiliated with middlemen sometimes travel up to 200 km to reach the city. Certain vegetables were even found to travel over 1,000 km from northern India.
For most other cities, such mapping remains absent, due in part to the informal and fragmented nature of supply chains and the lack of institutional attention to urban food planning.
Staple grains were found to reach Chennai from further afield. While some rice is sourced from Tamil Nadu’s delta districts, much of it arrives from states like Andhra Pradesh, Haryana, Delhi, Assam, and West Bengal, with brokers linking producers and Chennai-based millers. Wheat is mainly procured from Punjab, Madhya Pradesh, and Uttar Pradesh through similar channels. Pulses come from a mix of local sources and distant states such as Delhi and Haryana, as well as from international suppliers including the US, Canada, Australia, and Mozambique.
The city’s meat supply is more decentralised. Poultry, Chennai’s most consumed meat, is brought in from Tamil Nadu and nearby southern states, often through vertically integrated systems where companies provide chicks, equipment, and market access to local growers. Mutton, the second most popular meat, is transported over 2,000 km from states like Andhra Pradesh, Rajasthan, and Maharashtra, while beef typically comes from Kerala. Fish arrives not only from the Coromandel Coast but also from other coastal regions, thanks to improvements in cold storage infrastructure.
Projects like Who Feeds Chennai? offer a rare glimpse into how food reaches an Indian city. For most other cities, such mapping remains absent, due in part to the informal and fragmented nature of supply chains and the lack of institutional attention to urban food planning.
Around the world, city governments are increasingly recognising the importance of understanding and managing how food circulates through urban systems. A leading example is the Milan Urban Food Policy Pact, a global agreement signed by over 250 cities such as Milan, Nairobi, Rio de Janeiro, Seoul, Toronto, New York City, Dakar, Melbourne, and Amsterdam. Launched in 2015, the pact has supported initiatives worldwide to map food flows, strengthen urban–rural linkages, reduce waste, and improve access to nutritious food through public procurement and community-based programs. The Indian cities of Bhopal, Indore, Jammu, Panaji, Pune, Rourkela, Sagar, and Ujjain are also signatories. However, there is little publicly available information on whether these cities have undertaken detailed mapping of their food systems.

Also read: The circular bioeconomy movement can change how we see waste
As urban centres expand, they draw food, water, labour, and land from their margins, reshaping both agricultural production and everyday life. In the National Capital Region, rising urban demand has led to significant changes in land use in peri-urban regions, especially in Haryana. Farmers are increasingly turning to high-value crops like fruits and vegetables, aided by state support for polyhouse cultivation, horticulture promotion, and improved market access. These shifts are not only transforming cropping patterns but also strengthening local supply chains that feed the growing urban population.
However, risks remain: many smallholders face insecure tenure, erratic access to water, and volatile market conditions that limit long-term investment. As real estate interests encroach and cultivation becomes more marginal, benefits from intensified production are unevenly shared. Without more inclusive governance and safeguards for farming livelihoods, these shifts may deepen existing inequalities.
What enables economic survival in the short term may be contributing to long-term health and ecological decline.
In Bengaluru’s peripheries as well, food production has shifted away from traditional crops like millets and pulses towards high-value and high input-demanding crops like baby corn, mulberry, cattle fodder, as well as lawn grass. In particular, the rise of lawn grass cultivation for Bengaluru’s landscaping industry exemplifies a form of extractive agriculture that is ecologically damaging, socially disconnected, and diverts land that could otherwise be used to grow local food crops.
As a result of the city’s struggles with fresh water supply, agriculture in Bengaluru’s southern periphery depends on untreated or partially treated wastewater for irrigation. This has allowed farmers to cultivate year-round, boosting incomes and enabling diversification. But this practice is not without pitfalls. Vegetables and milk from these zones have tested positive for heavy metals, and residents report high rates of waterborne and skin-related illnesses. What enables economic survival in the short term may be contributing to long-term health and ecological decline.
Also read: The promises—and perils—of Indian aquaculture
Informal food networks, which take the form of streetside vendors and fish mongers, are central to how Indian cities eat. Unlike in many other parts of the world, large supermarket chains have failed to replace them, finding it hard to compete with the accessibility, affordability, and trust built into these local systems of provisioning. Though often overlooked in policy, informal food networks form a critical part of urban infrastructure, enabling both food access and livelihoods.
In cities like Mumbai, the informal food sector has been deeply shaped by the city’s history as an industrious port. Today, it is home to vibrant food networks that operate beyond the bounds of formal municipal governance but with a high level of coordination in how space and money are used.
Neighbourhoods like Dharavi, often reduced to shorthand for poverty or overcrowding, are also hubs of food processing, retail, and distribution. Dabbawalas, meanwhile, transport home-cooked lunches to offices across the city with remarkable precision, weaving through trains and traffic in one of the world’s most complex logistical systems.

Yet these systems remain precarious, and their workers vulnerable. Most vendors lack legal status, secure space, or access to basic infrastructure like clean water and waste disposal. Periodic evictions and restrictive regulations, often justified through concerns about hygiene or congestion, displace the very actors who make urban food access possible. These pressures are intensified by social hierarchies. Gender, caste, and migrant status influence who gets access to vending locations, how municipal authorities respond, and who bears the brunt of enforcement.
Kolkata offers a slightly different story. With over 3,00,000 vendors working across the city, street vending is just as widespread as other metropolitan cities, but more deeply tied to local politics. Over the years, hawkers have formed strong unions and built enduring ties with political parties. These relationships have allowed them not only to survive but also to resist eviction and, at times, gain influence over decision-making processes.
However, this visibility brings its own complications and power struggles. In many areas, clientelist politics now shape urban spaces wherein local leaders offer protection in exchange for votes. This means that basic services, rights, and fair treatment often depend on political loyalty rather than formal legal protection.
In 2014, India passed the Street Vendors Act, a national law aimed at recognising and protecting the rights of street vendors. It called for detailed surveys to register vendors, the creation of designated vending zones, and restrictions on evictions without due process. The law was intended to bring dignity and security to informal food work. But more than a decade later, implementation remains limited. Other kinds of food workers such as food delivery staff and domestic cooks also remain on the margins of labour protection, often navigating long hours, low pay, and few avenues for redress.
Also read: Can India’s traditional knowledge future-proof its food system?
As of 2025, urban food policy in India remains inconsistently implemented and disproportionately influenced by upper and middle-class interests, with little recognition of the informal actors who play a central role in enabling food access. A more inclusive approach must look beyond city centres and engage the wider geographies that feed them.
At a time when cities around the world increasingly turn to food imports to ensure food security—often adding to climate change—it is all the more important for India to draw on its rich biodiversity and traditional agricultural knowledge to meet urban food needs through domestic production.
Importantly, what becomes clear from examining India’s urban food landscape is that the path to improving it does not lie in replacing informal networks with privately led or corporate-controlled models. Rather, it lies in recognising that these networks of small traders, transporters, vendors, farmers, and millers form the foundation upon which urban food access depends. Far from being obsolete, they are resilient, adaptive, and deeply embedded in the country's social and economic life.
However, ensuring the rights and protections of those engaged in informal food work is not a call for deregulation, but for thoughtful, context-sensitive governance that values and safeguards these actors while addressing gaps in infrastructure, food safety regulation, transparency, and equity. Without such a framework, efforts to formalise or privatise the food economy risk excluding those who already deliver affordability and access to the majority of urban residents.
At a time when cities around the world increasingly turn to food imports to ensure food security—often adding to climate change—it is all the more important for India to draw on its rich biodiversity and traditional agricultural knowledge to meet urban food needs through domestic production. As a result of the country’s geographic and climatic diversity, a one-size-fits-all approach to urban food planning is unlikely to work. Policies must instead reflect regional specificities. Equally important is the need to curb corporate concentration in the food sector so that access to nutritious and affordable food is not limited to elites but extends to the working class. Encouraging the consumption of locally sourced foods through price incentives and public awareness can help align urban diets with regional food systems, supporting both sustainability and equity.
Artwork by Alia Sinha
{{quiz}}

Proteins are made of 20 building blocks. Your body only makes 11; the rest are on your dinner plate
Editor's Note: From grocery lists, to fitness priorities, and even healthy snacking, protein is everywhere—but do we truly understand it? In this series, the Good Food Movement breaks down the science behind this vital macronutrient and its value to the human body. It examines how we absorb protein from the food we consume, how this complex molecule has a role to play in processes like immunity, and the price the Earth pays for our growing protein needs.
Why has protein suddenly become the global poster child for modern nutrition? From nutritionists, to scientists, to artificial intelligence, everyone is invested in this macronutrient. In fact, one of AI’s biggest biology puzzles has become understanding how proteins fold into their unique 3D shapes.
Proteins are essential to our bodies. They build muscle, carry oxygen, fight infections, digest food, and even help our brains think. Essential components like enzymes, haemoglobin, hormones, muscles, and keratin—that constitute our organs, skin and hair—are made up of protein. The human body has over 20,000 protein-coding genes (segments of DNA that contain instructions on how to make proteins), and each protein serves a purpose.
But…what are proteins exactly?
The ways in which they fold (twist, curl and arrange themselves in 3D) determines what they eventually form, and how they function in the body—like enzymes, hormones and antibodies, among others.
Proteins are long chains made up of smaller molecules called amino acids. Think of amino acids like LEGO blocks—there are 20 kinds, and you can snap them together in endless ways to build thousands of different proteins. The ways in which they fold (twist, curl and arrange themselves in 3D) determines what they eventually form, and how they function in the body—like enzymes, hormones and antibodies, among others. But predicting this folded shape just from the sequence of amino acids is a complex affair.
(Note that proteins are infinitely varied and intricate—and this short explainer only scratches the surface. It’s like trying to describe the entire Internet using a sticky note. But hey, we’re trying.)
Also read: Protein’s seen and unseen benefits: How it affects metabolism, muscle repair
We need to know which amino acids build the protein molecule before predicting how it may fold. This is known as protein sequencing. Why is this important? To understand how a protein functions, how it interacts with other molecules, and how mutations may cause it to malfunction.
For instance, a single amino acid change in the haemoglobin protein leads to sickle cell disease, altering the shape and function of red blood cells. Insights like these help researchers develop targeted medications, study genetic disorders, and even design synthetic proteins from scratch—such as enzymes that break down plastic, or lab-made antibodies used in cancer immunotherapy. Essentially, protein sequencing helps understand life on a molecular level.
Insights like these help researchers develop targeted medications, study genetic disorders, and even design synthetic proteins from scratch—such as enzymes that break down plastic, or lab-made antibodies used in cancer immunotherapy.
The quest to sequence this macronutrient stretches back centuries. As early as 1789, French chemist Antoine Fourcroy noticed that substances like albumin, fibrin, and gelatin shared similar properties, though back then they were still called ‘Eiweisskörper’ (literally, ‘egg-white bodies’). A few decades later, in 1819, Henri Braconnot managed to isolate the first amino acids, leucine and glycine, from natural sources—hinting at the building blocks behind proteins.
The word ‘protein’ itself was coined in 1838 by Dutch chemist Gerardus Johannes Mulder, rooted in the Greek ‘of first importance.’ But it wasn’t until the 20th century that things really took off.
In the early 1950s, Frederick Sanger cracked the amino acid sequence of insulin, proving for the first time that proteins have precise, genetically determined structures. Around the same time, George Palade discovered ribosomes—the workers in our cells that assemble proteins based on instructions from our genes. Then in 1958, John Kendrew used X-ray crystallography to unveil the first detailed 3D structure of a protein—myoglobin from a sperm whale—ushering in the age of structural biology.
Fast-forward to 2020, DeepMind’s AI tool AlphaFold accurately predicted protein’s myriad 3D shapes from amino acid sequences—something that took labs years to figure out. In 2021, it released structures for over 200 million proteins (essentially covering every protein known to science today), transforming the way we understand what our bodies are made of.
Also read: Whey to go: A complete guide to protein
Okay, quick recap. Remember those 20 amino acids that are the building blocks of protein? Out of these, 9 are ‘essential’; your body can’t make them. You have to get them from food. The other 11 are ‘non-essential’; your body can process them from other nutrients like carbohydrates and fatty acids.
This is why pairing foods matters. If you're vegan, aim to combine grains, legumes and nuts/seeds across meals. A classic example is rajma and rice, or the old American favourite, a peanut butter sandwich. If you're vegetarian, adding a little dairy simplifies things a lot.
Not all protein sources give you all 9 essential amino acids. Foods like meat, fish, eggs, dairy are called complete proteins because they check all the boxes. But most plant-based proteins are incomplete, which means they’re missing one or more of those 9 essential amino acids.
This is why pairing foods matters. If you're vegan, aim to combine grains, legumes and nuts/seeds across meals. A classic example is rajma and rice, or the old American favourite, a peanut butter sandwich.
If you're vegetarian, adding a little dairy simplifies things a lot. Some go-to combinations include moong dal cheela (soaked mung bean crepes) and pairing it with curd or yogurt. Another excellent option is chole (chickpea curry) served with whole wheat roti and a side of buttermilk, offering a balanced and protein-rich meal. Similarly, moong dal khichdi paired with lightly grilled paneer cubes creates a wholesome lunch packed with protein and essential nutrients.
What happens if you don’t get enough protein? Well, protein deficiency hits hard and fast. You feel weak, tired and your immune system tanks – you catch colds quicker, and your injuries are slower to heal. In children, physical growth becomes stagnant and their brains lag behind. In extreme cases, it can lead to kwashiorkor, a condition where children have bloated bellies, thin limbs, and severe health problems.
Also read: Is your body low on protein? Signs and impacts of a deficiency
{{quiz}}
Please try another keyword to match the results
