The virus, though deadly, is unlikely to lead to a pandemic. Yet in the absence of a ready vaccine, being cautious is important






Late in December 2025, two healthcare workers in West Bengal’s North 24 Parganas district developed symptoms of a severe viral infection. On 13 January, the National Institute of Virology’s laboratory confirmed that these were indeed the Nipah virus. Though rare, the virus invokes deep fear globally; several of India’s neighbours have already started screening Indian visitors as a precautionary measure. Why does the virus induce fear, and what is its true risk potential?
The fear surrounding the infection stems from two main causes: the lack of a licensed treatment or vaccine, and the difficulty in early diagnosis.
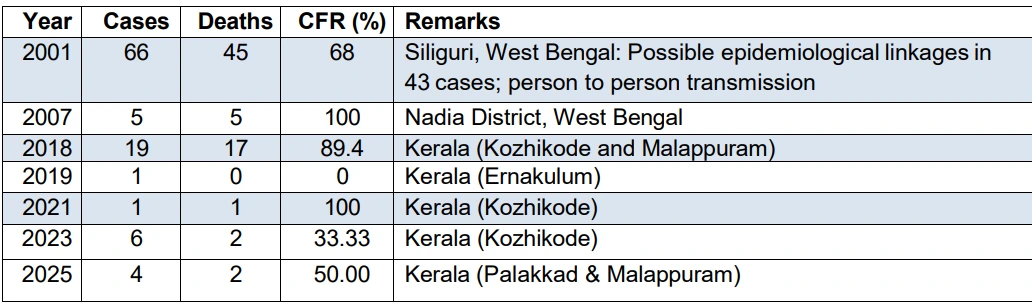
The Nipah virus is a zoonotic virus, i.e. it is transmitted to humans through animals. The virus can jump to humans in two ways: through contact with the saliva or other bodily fluids of the natural hosts of the virus like fruit bats or flying foxes, or through intermediary hosts (usually pigs or other humans) who have been infected. The virus, first identified in Malaysia in 1999, has only affected five countries so far, all from Southeast Asia. India has had 8 outbreaks over the past quarter century, including the latest one. Globally, there have been 754 cases and over 435 deaths since the virus was first identified.
Symptoms and treatment
The infection has an incubation period of three to 14 days—this is the time interval between the virus’s entry in the body and the first appearance of recognisable symptoms. While some people may remain asymptomatic, most show at least mild symptoms like fever along with symptoms involving the brain (such as headache or confusion), and/or the lungs (such as difficulty breathing or cough). Patients with mild symptoms can make a full recovery. However, if the infection becomes severe, the symptoms become neurological, and indicate encephalitis—that is, a swelling of the brain. Encephalitis and seizures usually progress to a coma in 24 to 48 hours. Patients with severe infections are also likelier to spread the infection.
For those who survive, recovery is slow, and for some, neurological symptoms persist for years because of the way the infection impacts brain cells. This makes rehabilitative care critical for patients on the mend. The case fatality ratio (CFR), that is the percentage of patients who will die, varies widely. The WHO places it in the range of 40% to 75%, but India has reported CFRs both below and above these figures. In the absence of any known cure, treatment for patients is limited to intensive supportive care, including rest, hydration, and treatment of symptoms as they occur. Still, hospitalisation is important to monitor the way the disease affects a patient’s organs, and to control transmission.
The fear surrounding the infection stems from two main causes: the lack of a licensed treatment or vaccine, and the difficulty in early diagnosis. Though a vaccine is under trial, and some drugs have worked in limited capacities, none of these are officially approved by the WHO yet. Early diagnosis is difficult for many reasons. Firstly, the symptoms of mild infection are very similar to a regular viral infection. Secondly, the testing process is sophisticated. This leaves only a handful of institutes in the country equipped to test for Nipah virus. Of them, the Indian Council of Medical Research (ICMR) has authorised only one institute—National Institute of Virology (NIV) in Pune to confirm cases. This is because NIV Pune is the only Bio-Safety Level 4 (BSL-4) laboratory in the country. The biosafety level certification is also important to contain the samples and ensure that biowaste is disposed of safely after testing.
Also read: How drug-resistant tuberculosis is bringing life to a halt in India
Prevention
In India, only bat-to-human and human-to-human transmissions have been identified. Bat-to-human transmissions are generally caused by consumption of food that is contaminated by the blood, urine, or saliva of fruit bats. In West Bengal, especially, outbreaks have been linked to the consumption of raw palm date sap (Khejur Ras) and coincide with the harvest season for the sap (December to May).
The precaution, then, is to thoroughly wash and peel fruits before consumption, especially if one lives near areas with a bat population. If a fruit has bite marks, discard it. And in the case of palm date sap, boiling it to form nolen gur or patali gur before consumption can ensure safety.
The Nipah virus is not airborne; human-to-human transmission happens through contact with bodily fluids or contaminated bodily tissue. Contaminated tissues can refer to tissues collected during testing or tissues discarded during surgical processes while treating any organs affected by the virus. This places caregivers, healthcare workers, and even those conducting burial/funeral rituals at risk. Preventative measures include assigning patients to single rooms, wearing protective gear like gloves while caring for or visiting patients, and washing hands after. Hospitals and laboratories also have to follow strict procedures for handling and disposing tissues to prevent transmission.
The virus, though deadly, travels in a very tight circle and has been vigilantly managed.
That said, the Nipah virus is unlikely to lead to a pandemic. It typically has a reproduction number of less than 1. This figure indicates the expected number of secondary infections stemming from a primary infection, signalling that its tendency for human-to-human transmissions is low.
On 26 January, 2026, India notified the WHO about the two Nipah virus positive cases. They also confirmed, after testing 190 contacts for the virus, that no further cases have been detected. Out of the two patients, the second case has shown clinical improvement, while the first case remains under critical care.
The virus, though deadly, travels in a very tight circle and has been vigilantly managed. Outbreaks have been linked to habitat disruption of the host bats, and are likely to happen again in areas where urban spaces are replacing woodlands. Even as vaccines are being developed, being vigilant, maintaining hygiene, and focusing on prevention remains the best cure.
Also read: Add crisis to cart: Why instant delivery and antibiotics don't mix
Explore other topics
References




.avif)

.avif)