Mistrust leads to delayed diagnosis and treatment, further endangering their health






Keshwari is a 32-year-old married woman who is employed as a sanitation worker. She was brought to Delhi from the Bhagalpur village in Bihar, to earn a living and support her family. While in Delhi, she was diagnosed with kidney stones by her family doctor and advised to get surgery.
In her neighbourhood’s Mohalla Clinic, Keshwari sits back after another spell of dizziness—a frequent sign of her weakness. Her surgery was extremely expensive, and treatment had been visibly delayed. But she is not in the clinic for herself—she needs to get her son vaccinated. She doesn’t trust the city’s doctors. “There’s no support here; who would help if something went wrong?” Keshwari doesn’t plan on returning to Bhagalpur in the near future. As for her health, it is another sacrifice she is willing to make.
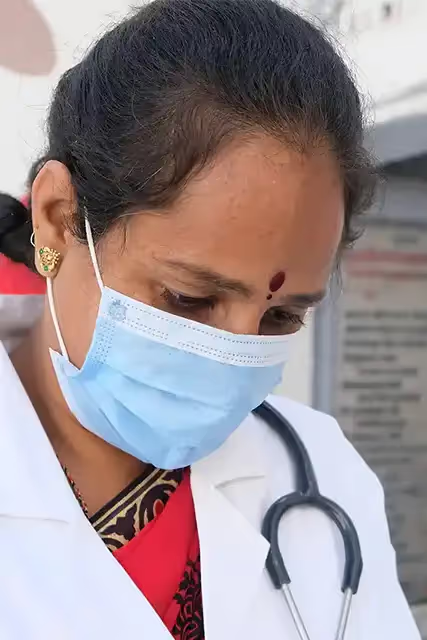
Haseena Begum, a 40-year-old married woman, has worked in a public hospital in Malviya Nagar all through the COVID-19 pandemic. Last year, after four months of excessive bleeding during her menstrual cycles, Begum knew something wasn’t right. She took the day off from work and travelled to a government hospital in South Delhi, still bleeding heavily. “ I didn’t want to go,” admits Begum. “I am shy and I don't like the way they touch me.”
When she did see the doctor, her experience didn’t quiet her anxieties. “She barely looked at me. I told her I was uncomfortable with getting a check-up, I had never had a doctor [gynaecologist] check me before. She started to scold me, saying that I was wasting her time.” Eventually, Begum went to a local pir (spiritual guide), who gave her ‘healing water’ to alleviate her symptoms; she hasn’t been to a doctor since. When this writer asks her why, she says, “Humein aur kuch nahi chahiye, sirf pyaar se baat karein. [I’m not asking for much, only to be addressed kindly].
These incidents are not isolated.
For the first time in ten years, the rate of hospitalisation in India has fallen. Data from National Sample Surveys conducted in the last decade show that in 2014, India had 31.5 hospitalisations for every 1,000 people. By 2017-18, this number fell to 28. This may seem optimistic, but experts caution that it only points to a decline in the utilisation of public healthcare services. Fewer people are visiting public healthcare centres—a reality complicated by another gaping statistic: fewer women are seeking medical treatment from these centres.
More women are paying out-of-pocket at private healthcare centres, raking in debt. They are turning to alternative medicine, or simply avoiding diagnosis and treatment until it's too late.
The skewed sex ratio of patients in public hospital registers like AIIMS point to ‘missing women’. While these realities have played out in the foreground, cancer-related mortalities in India have increased specifically among women in the last decade.
So, where do the ailing women of this country go? More women are paying out-of-pocket at private healthcare centres, raking in debt. They are turning to alternative medicine, or simply avoiding diagnosis and treatment until it's too late. This is happening for myriad reasons, many of which culminate into one glaring truth: women are losing trust in Delhi’s public healthcare system.

In a study conducted jointly by AIIMS—the largest tertiary care hospital in India—and the Harvard Medical Centre in 2016, the authors went through the outpatient records at AIIMS for the entire year of 2016, and found an eerie gap. Only 37% of the patients were women, against 63% men. This suggests a sex ratio of 1.69, whereas the average sex ratio of the populations that they served was 1.09. Ideally, both these numbers should be consistent. The data showed a whole chunk of ‘missing’ women, suggesting that there may be a significant percentage of women who just don’t visit the hospital at all—and don’t get access to healthcare in the process.
Apart from systemic issues of financial dependence, community taboos, and a general lack of awareness about women’s bodies, there seems to be another reason why women remain inconsistent in accessing healthcare. A factor that persists even after these barriers are removed: a lack of trust grounded in disrespectful care. Much of this begins with the dents in the country’s health infrastructure.
The disappearance of primary healthcare
For instance, an over-dependence on secondary and tertiary healthcare institutions have left urban populations bereft of local clinics, where they could build trust with the medical staff.
In Delhi, schemes like the Mohalla Clinic programme—launched by the Aam Aadmi Party government in 2015—had helped bridge this gap to an extent. Studies show that these clinics did lead to increased annual patient visits and relief for larger public health institutions, especially with respect to patients from lower-income groups. But with news of recent closures of the clinics, the gaps in primary healthcare may widen once again.
Public health experts suggest that the issue is the paucity of public healthcare at the primary level, which leads to secondary and tertiary institutions like AIIMS and Delhi’s Safdarjung Hospital absorbing the pressure. “Primary Health Centres (PHCs) were part of the rural imagination, and when these areas became urbanised rapidly, such centers couldn’t cater to the high density of the population. The urban primary health care system requires some rethinking,” says Dr. Nandita Bhan, a professor at the OP Jindal’s School of Public Health in Sonipat.
Despite being the national capital, Delhi’s public healthcare system is a microcosm of the country’s medical framework—overwhelmed, stretched for resources, and unevenly distributed.
Primary healthcare in Delhi was envisaged with schemes like the Mahila Mohalla Clinic programme. They intended to ease access of patients, thus also increasing detectability of health issues—particularly women’s cancer and other gynaecological issues.
However, as suggested by a 2017 report, only about 2.9% of the 1020 women studied had undergone cervical cancer screening in the capital. Mridu Gupta, CEO of CAPED India, a cancer awareness non-profit in Gurgaon, suggests that women’s lack of access to healthcare isn’t linear. “For women to have trust, they must have some autonomy over their bodies—dependence on male members of the family to even visit clinics or get tested and, a lack of awareness about their own bodies often pushes them to first try out household nuskas to manage symptoms before they even approach a doctor.” The situation worsens when hospitals are ill-equipped to care for women, lacking female doctors or adequate time and resources to effectively deal with these maladies. “Especially when women present with heavy bleeding or extreme pain, male doctors tend to dismiss them as simply period symptoms,” Gupta adds.
Despite being the national capital, Delhi’s public healthcare system is a microcosm of the country’s medical framework—overwhelmed, stretched for resources, and unevenly distributed. Dr. Bhan adds, “With women’s health, we often see delays in testing and formal diagnoses since they choose to access informal or traditional care facilities which may not be fully medically adept at handling their conditions.”
Also read: How food inflation is squeezing Indian households
Trust and reproductive health
Research on disrespectful care in India has only recently come to be explored, focusing on maternity care in the North-East and Uttar Pradesh. Sonam and Babita, two government sweepers in their late 30s, have been residents of Sardar Nagar in West Delhi all their lives. After the deliveries of their children at a public hospital in the city, the duo has not stepped foot in the institution again. “It was my first child and I was clueless—all I was told was that I should come to the hospital when I had labour pains. They didn’t even do an ultrasound to see that my baby was stuck in the umbilical cord; eventually I needed a cesarean delivery,” Babita claims.
These experiences left them feeling disrespected and uncared for. The hours after their deliveries did not provide much relief either. Without stitches, in pain and covered in blood, they lay there for hours. Since then, both Sonam and Babita prefer to go to private clinics in their neighbourhood, when they can afford it. Their examples echo a larger trend: nearly 79% of outpatient visits, particularly in urban areas, are catered to by private facilities—leading to high out-of-pocket expenditures. For many women, the cost of being heard was a cost worth bearing.
Dr. Jyoti Sharma of the Indian Institute of Public Health (IIPH) raised the issue of screening for cervical and breast cancer. “We see women being diagnosed in the second or third stage, after having heavy bleeding for months.” According to the National Health Profile 2019, there were approximately 60,078 deaths due to cervical cancer in India in 2018. Additionally, an estimated 87,000 women died from breast cancer in India in 2020, with Delhi accounting for the highest number of cases in North India. Dr. Bhan added, “This may be due to better screening at tertiary facilities, and more women coming to the capital city for diagnoses, but the taboo around cancer also surrounds the issue of delayed access.”
For many women, the cost of being heard was a cost worth bearing.
If financial access and the lack of proximity aren’t enough, there’s also a fear of cancer. “There’s the attached social stigma which discourages women from going to the doctor. Women with cancer are made to avoid social gatherings or joyous occasions. Women’s health is already seen as expendable, often being seen as less valuable than the health of children or the man of the house,” says Dr. Bhan.

There’s also a false association with the hereditary nature of some kinds of cancer, pushing women to avoid diagnoses and save their children from social isolation. Another stigma that can be extremely dangerous links preventative care like the HPV vaccine to a woman’s sexual health—and this may cause many women to avoid the inoculation despite awareness, putting them at a higher risk of cervical cancer in the future.
Mridu Gupta also says that detection for most women’s health issues is often delayed, from endometriosis to cancer. “The only solution to mistrust is communication, but doctors are so overworked that information to the patient is relayed on a need-to-know basis.”
The brewing distrust in the medical profession has deeper roots. Dependent on community experiences, traditional cultural cures, and social stigma, many people avoid seeking conventional medical care. But this is exacerbated when it comes to women in urban areas, who are also limited by a lack of financial confidence, proximity, limited independence, and awareness. Operating within these limitations, it becomes necessary for governments to not only develop means of access, but also make them easy. For women, effective care involves not just the removal of physical barriers to healthcare access, but also fostering relationships of care and respect between patients and doctors.
{{quiz}}
References



.avif)

.avif)