Antimicrobial resistance is making infections tougher to treat






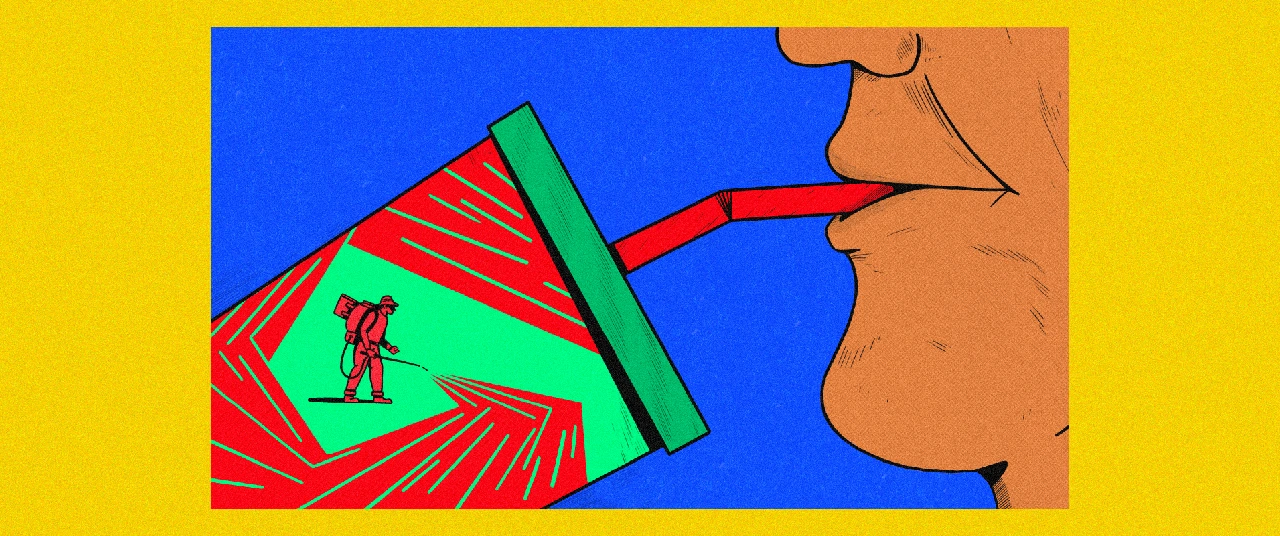
Antimicrobial resistance, or AMR, is a fast-evolving threat to global health systems. According to the World Health Organization (WHO), AMR occurs when bacteria, viruses, fungi, and parasites no longer respond to antimicrobial medicines as they develop drug resistance.
In many wealthy countries, doctors frequently prescribe antimicrobials even when they aren't necessary, according to a paper published in the United States National Center for Biotechnology Information. Meanwhile, in developing nations like India, these drugs are often readily available over the counter, leading to rampant misuse.
A study in The Lancet Regional Health — Southeast Asia highlighted India's high consumption of broad-spectrum antibiotics, which should be used sparingly due to their wide-ranging effects. The journal JAC—Antimicrobial Resistance reported that antibiotic misuse varies significantly across India, with poorer states showing lower rates of consumption, likely due to limited access rather than prudent use. This misuse breeds superbugs—pathogens armed with resistance genes that render treatments ineffective. As a result, common infections become increasingly difficult, if not impossible, to treat.
According to a report published by the Indian Council of Medical Research, a big chunk of patients in India may no longer benefit from carbapenem, a powerful antibiotic used in critical care settings to treat pneumonia and septicemia. The resistance isn't limited to bacteria. Fungal pathogens like C. parapsilosis and C. glabrata are showing increasing resistance to common antifungal medicines such as fluconazole.
Unfolding catastrophe
In 2019 alone, drug-resistant infections claimed 1.27 million lives globally. The United Nations warns that by 2050, this number could soar to a staggering 10 million annual deaths.
According to an article in the United States Centers for Disease Control and Prevention (CDC), antimicrobial-resistant infections that require the use of second- and third-line treatments can harm patients by causing serious side effects, such as organ failure, and prolonged care and recovery, sometimes for months.
The article further says that resistance also comes in the way of a person’s ability to fight infections using antibiotics during treatments/procedures, including joint replacements, organ transplants, cancer therapy, and chronic diseases like diabetes, asthma, and rheumatoid arthritis.
According to the United Nations Environment Programme (UNEP), AMR could shave off USD 3.4 trillion from global annual GDP and push 24 million more people into extreme poverty in the next decade. The UNEP also warns that by 2050, up to 10 million deaths could occur annually due to drug-resistant infections globally.
Beyond human health
The misuse of antimicrobials extends beyond humans, affecting food-producing animals and aquaculture. The widespread use of these drugs to promote growth and prevent disease has led to resistant bacterial strains that can spread to humans through direct contact, consumption, or the environment.
While AMR drivers are universal, its impact is disproportionately severe in low- and middle-income countries, as noted by the WHO. Here, the overuse of non-prescribed drugs is more prevalent, exacerbating existing inequalities as healthcare costs rise and agricultural productivity falls.
Charting a new course
Recognising the gravity of AMR, scientists and policymakers advocate for a multi-faceted approach. Improved surveillance is crucial, as highlighted by the United States Library of Medicine. Gaps in data on key microbes hinder our understanding of AMR trends, making it essential to establish standardised methods and definitions for tracking resistance.
Hospitals must improve infection control measures, while public education campaigns can help curb antimicrobial misuse. The Federation of European Microbiological Societies (FEMS) suggests that effective public awareness campaigns could cut antimicrobial prescriptions by 36%.
In agriculture, reducing antimicrobial use in livestock and developing new drugs to combat superbugs is imperative. The UNEP emphasises the environment's role in AMR's evolution and spread, advocating for a 'One Health' approach that recognises the interconnectedness of humans, animals, plants, and ecosystems.
A call to action
For the 'One Health' strategy to succeed, global organisations and governments must prioritise AMR as an international concern. The time has come to place this threat at the forefront of the global political agenda, acknowledging that addressing AMR is not just a scientific or medical issue but a societal imperative that demands coordinated action from all sectors. Only by acting decisively can we hope to avert the looming health crisis and safeguard future generations from the devastating impact of drug-resistant infections.
Explore other topics
References