Despite global health organisations and laws vouching for exclusive breastfeeding for the first six months, formula is making a dent in infant nutrition






Across delivery rooms in India, whether in public or private hospitals, newborns are increasingly being fed formula as their first meal, often without parental consent. This trend is not accidental. From the lack of institutional and infrastructural support for breastfeeding, to marketing by formula brands, to healthcare professionals advocating for formula milk (FM), infant formula is on the rise in India. This reality unfolds even as it poses deep threats to child health, maternal well-being, and inevitably, public nutrition.
A report from The News Minute details the experience of Vidya Sanap, a 32-year old researcher at IIT Bombay, who was eager to breastfeed after a C-section delivery, but when she asked the nursing staff for help, she was chided. “Your breast milk won’t run out if you don’t feed immediately,”—this is how Sanap remembers the nurses’ response. Another report in Quartz talks about another new mother’s first experience with breastfeeding: Sanika Chawla had delivered a healthy boy at a private hospital in Bengaluru. However, she didn’t get to hold him for several hours. Much to her chagrin, he had already been fed formula for his first meal.
These are just some among numerous examples in maternity wards, where babies are being whisked away by nursing staff and initiated on formula, against the mother’s wishes. What drives this breastfeeding-versus-formula turf war across Indian infant care?
Mother’s milk
The World Health Organization (WHO) recommends that infants be exclusively breastfed (EBF) for the first six months. Continued breastfeeding is recommended until a child turns two, with complementary foods being introduced after six months. Medical research has drawn countless links between early breastfeeding and its positive impact on both infant and maternal health. Lactation experts confirm that colostrum—the thick yellow liquid that is produced by the mother during pregnancy—is loaded with antibodies and immunoglobulins that boost infant immunity.
UNICEF advocates breastfeeding within the first hour of birth, but government data shows that only about 42% of all Indian babies have that healthy start.
Mothers also transmit good bacteria, which live in the infant’s gut, helping digest food and boosting their immune system. Breastfeeding significantly lowers infant mortality and risks of gastrointestinal disease and obesity in later life. Additionally, mothers who breastfeed have lowered chances of ovarian and breast cancer, Type 2 diabetes and cardiovascular disease. This is especially pertinent in countries like India with high rates of infant and neonatal mortality—27 infant deaths and 19 neonatal deaths for every 1000 live births in 2021.
UNICEF advocates breastfeeding within the first hour of birth, but government data shows that only about 42% of all Indian babies have that healthy start. There are legitimate reasons as to why breastfeeding isn’t always a viable option; not every newborn takes to the nipple immediately, or has a breastfeeding mother. Sometimes, new mothers also experience lactation failure.
The early makers of infant formula recognised this. The first known commercial infant formula was a cow milk-based formula made by chemist Justus von Liebig in Germany in 1865. Until then, many gave their infants other substitutes like homemade evaporated milk, and ‘pap’, a bread-and-water mush, from hard-to-clean utensils teeming with bacteria. Others employed wet nurses—women who were responsible for breastfeeding another’s child. Death rates were alarmingly high in the early 1800s, only two in three babies who weren't breastfed completed the age of one. The timing of Liebig's formula was opportune, and the appeal quickly spread beyond just women who couldn’t breastfeed. Liebig’s Soluble Food for babies (comprising primarily cow’s milk, wheat and malt flour and potassium bicarbonate) made commercial formula accessible and affordable.
Physicians in the 1960s and ‘70s (especially in the Global North) also began recommending these commercial formulas, making them more popular among mothers. However, an important detail to note here is that infant formula was developed as a substitute for breast milk, specifically for mothers who couldn’t breastfeed. Bridging a gap in infant nutrition was Liebig’s primary motive behind the development of formula.
And so it went, for a while: it seems like formula milk was mostly used on a case-by-case basis. What changed? What led to the formula boom?
Also read: The transformative potential of universal school meals
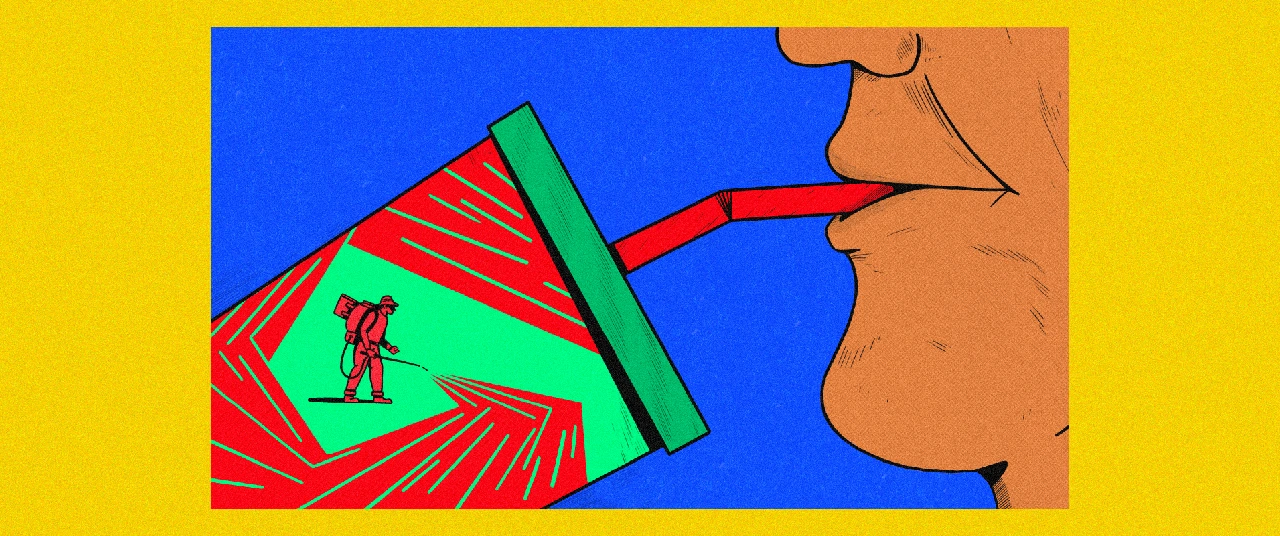
Formula’s vulture grip
For one, the introduction of formula dramatically transformed the workplace. For many new mothers who want to, or must return to work, formula is a lifeline—especially when taking extended time away can come at a real cost to their careers. Several studies mention that earning gaps increase after mothers return to the workplace once their maternity leaves end. One mother says formula helped both her and her baby adapt to a work routine: “I had to go back to work in three months, so I started topping up with formula in two months so that my supply would temper and my baby would get used to the bottle.”
According to the WHO, the global formula milk industry was worth $55 billion in 2022. It has also found that global breastfeeding rates have increased very little in the last two decades. Meanwhile, the sale of formula milk has more than doubled in the same period.
Evolution has carefully fine-tuned the ‘recipe’ for breast milk to optimise for both maternal and infant health. Infant formula is a manufactured breast-milk substitute, available in liquid or powder form. However, infants' intestines are not naturally designed to digest these, lactation consultant Manisha Gogri says. Different compositions make up different infant formula. A series of articles published by The Lancet in 2016 lists the risks, which include more episodes of diarrhoea and respiratory infection. Companies that make formula claim that long chain polyunsaturated fatty acids in formula milk are involved in the development of the brain, eyes and the nervous system. However, these statements have little substantiation in scientific literature.
India has one of the most stringent laws in the world against breast milk substitutes, detailed in the Indian Milk Substitutes (IMS) Act, enacted in 1992 and enforced in 1993. The Act regulates the production, promotion, and distribution of infant milk substitutes by prohibiting advertising, point-of-sale promotions, and free samples, while placing stringent labeling requirements on these products as well. It also restricts health workers and institutions from providing biased information. Despite this, under the pretext of offering a substitute in cases of “low breast milk supply,” a multimillion-dollar industry thrives, claiming to calm crying or fussiness and to keep babies more satiated.
However, the idea of new mothers having a ‘low breast milk supply’ may very well be a myth. In a detailed report from The Wire, Dr. Arun Gupta, chairman of Breastfeeding Promotion Network of India (BPNI), a national NGO to promote healthy breastfeeding practices, says that a mother can usually produce enough milk to feed her baby, but it is often a challenge to bring the supply forth and nurse the baby. A host of other factors affect this process: milk production and flow depends—the more a baby breastfeeds, the greater the demand for milk in the mother’s body. Suckling activates nerves that signal the body to release prolactin and oxytocin. Prolactin triggers the alveoli to produce milk, while oxytocin makes the tiny muscles contract, pushing milk from the alveoli into the ducts. The release of oxytocin is also sensitive to a mother’s mental state. Dr. Gupta says that predatory tactics by formula makers disrupt this, pushing mothers into believing they cannot produce enough. Since breast milk supply is contingent on how much the baby feeds, introducing formula also affects it.
India has one of the most stringent laws in the world against breast milk substitutes, detailed in the Indian Milk Substitutes (IMS) Act
In India, especially, women face heightened familial and social scrutiny on their choice to nurse and/or introduce formula. A blog outlines how this new mother felt cloistered by her family while feeding: “Every session of breastfeeding (basically, every two hours) was slowly unravelling into a nightmare, where I felt I had no control. My female relatives would surround the bed, one of them holding the baby, and others pressing my nipple and commenting on my milk supply. My husband and I felt very helpless,” she says.
“I was under tremendous stress and … unable to generate enough milk for my son, who was subsequently fed only cow milk and formula,” another mother says. Surveys have found how over 50% of nursing mothers cite both physical and emotional breastfeeding woes, including sore nipples and irritated skin, a reason why they may turn to formula, especially if they have more than one child. These stories have themes in common: mothers feel like they do not have enough information and support on either breastfeeding or formula. This makes them feel like they have to endure the journey alone, and even when they do turn to formula, it isn’t without guilt or a public questioning of their scruples.
.jpg)
And then there is the matter of breastfeeding among low-income populations: one could expect it to be higher, owing to the rising costs of baby formula. What emerges is a very counterintuitive conclusion. The pressure to return to work makes EBF for six months difficult for many mothers, and this is especially true for the urban poor, who–being part of the informal labour sector–virtually have no maternal care benefits. There are examples of FM companies having infiltrated low-income countries as well: they offer cheap samples at first, and then dramatically increase prices, further entrenching families in cycles of poverty. Formula is also expensive, and so, many families tend to stretch out a box for much longer. The unavailability of clean water in most Indian slums, too, risks infant health.
Also read: Food fortification 101: Can foods built in with nutrients counter malnutrition, deficiencies?
A public health crisis, exacerbated
If the IMS Act provides a solid legislative foundation, intervention by healthcare professionals is crucial to counter misinformation. Yet, the crisis is often exacerbated by the neonatal healthcare industry itself. A WHO survey on formula nutrition in 15 countries (excluding India) reported that 60% of women in Bangladesh and 45% in Nigeria had received a recommendation for formula from a qualified health worker. With birth rates declining in the West, countries like India and China have become primetime targets to boost formula sales. Another study across eight countries by the WHO and UNICEF—including Vietnam, China and Bangladesh—showed how formula marketing directly influences feeding decisions, despite the International Code of Marketing of Breast-milk Substitutes (1981). Apart from using a myriad of offline and digital marketing channels, formula companies also sought to alter medical professionals’ understanding of this breast milk substitute, since they had direct access to patients. Trusted brands have come under fire for promoting their products as ‘identical’ to breast milk.
Dr. Gogri says that one of the most common misconceptions that parents have about breast milk and formula is that they are equivalent in nutritional content.
Dr. Gogri says that one of the most common misconceptions that parents have about breast milk and formula is that they are equivalent in nutritional content. Dr. Armida Fernandez, former Head of Neonatology at LTGM Hospital, Sion (hereafter referred to as Sion Hospital), weighs in on how hospital staff are often complicit. “After birth, the baby should be put to the breast right away, because the more the baby sucks, the more milk will come in. In the first days, milk comes in very small quantities—sometimes just drops—and that is normal. Mothers need to be reassured that this is enough, since a newborn’s stomach is only about the size of a thumb,” Fernandez says. When the babies cry incessantly, parents panic and are led to formula as a quick-fix solution.
“Instead of keeping the baby on the mother’s chest and ensuring what we refer to as ‘skin-to-skin contact’, many hospitals put the newborn under a warmer and even give them a bath. Both these practices lead to rapid fluid loss,” Fernandez adds.
When asked about how formula is peddled in hospitals despite the IMS Act, Gogri underscores the basic fact that formula milk is, in the end, medicine. “Hospitals always stock FM containers, it is only advertising and promotion that is discouraged. Not all use of formula in hospitals can be attributed to malpractice or any malicious intent, really. More often than not, it's just a lack of awareness and negligible counselling about how important breastfeeding is in those early hours,” Gogri says. Many mothers aren’t aware of the benefits of breast milk, and even those who do, sometimes find themselves fighting back against their own caregivers.
Not all use of formula in hospitals can be attributed to malpractice or any malicious intent, really. More often than not, it's just a lack of awareness and negligible counselling about how important breastfeeding is in those early hours,” Gogri says.

In India, a lack of infrastructural as well as social support for mothers also prevails. A dearth of breastfeeding and pumping rooms in public spaces and the stigma around breastfeeding in public in the first place also explains why mothers turn to formula. Gogri says that BPNI has set up Hirkani Kaksha–rooms designated for breastfeeding and expressing milk–in Maharashtra. “Several rooms have been set up at bus stops and train stations across Maharashtra. Unfortunately, many of them are unclean and in various states of disrepair; some have even become dumping grounds for trash,” she says.
Breast milk banks may offer answers
Discouraging or banning formula milk is not the answer. Even the BPNI acknowledges that formula is an essential part of infant and young child feeding in cases of lactation failure. Brazil, which runs the world’s leading breast milk donation program, shows another path forward: one where mothers are encouraged to donate their milk to vulnerable infants who might otherwise depend on formula.
The need for human milk banks in India is immense. Each year, 2.7 crore children are born in the country, of which 75 lakhs have low birth weight and 35 lakh are preterm. A preterm infant requires at least 30 ml of milk—volumes that add up quickly across millions of births. Yet, infrastructure remains scarce: until 2013, only 8–10 milk banks existed, and even today metro cities average only 5–6 banks each.
Dr. Armida Fernandez pioneered Asia’s first milk bank at Mumbai’s Sion Hospital in 1989. When asked what the Sion Neonatal Intensive Care Unit (NICU) was like at that point, she says, “We were losing newborn babies because of diarrhoea and sepsis, and one of the reasons was a feed of formula. I realised that if we had to stop the infection at source, we had to move to breast milk exclusively. And to ensure a continuous and safe supply of human milk, we needed a human milk bank.”
At the time, the concept of milk banks was alien, and Fernandez faced a lot of distrust and suspicion. “I never faced skepticism from the mothers themselves. Many mothers were ill and needed milk to support their babies, and others in the ward volunteered to be informal wet nurses for strangers’ babies. Once, a new mother who was also a resident at the hospital fed a baby who had tetanus, and it survived only because of her,” she adds.
Himani Khandekar, the manager at the milk bank, or the Comprehensive Lactation Management Centre (CLMC) at Sion Hospital, Mumbai, says that the objective is to ensure that infants are exclusively breastfed until their discharge. The reality of operating a milk bank, however, is grim and laborious. “Our supervisors and counsellors are scattered across the NICU, TCU (transitional care unit), and the post-natal care units, where mothers and babies rest after discharge. All these areas have separate breast milk pumping stations. The staff make individual rounds, personally going from bed-to-bed, training mothers in better breastfeeding practices, helping infants to latch.,” Khandekar says.
All mothers who are admitted in the hospital undergo an evaluation of their medical history, a serological testing of their milk and a physical examination of the breasts. When patients pass this screening, they are encouraged to be donors. “Counsellors help mothers understand the benefits of donating: it relieves their fullness and pain, can help other vulnerable infants, and actually increase their production as well, quite contrary to the myth of ‘running out.’”
The milk from these three different areas is pooled and divided equally into three equal aliquots to be fed into the Sterifeed—a fully-automatic pasteurizer capable of holding 36 bottles of 250 cubic centimetres of milk. The milk undergoes a heating cycle, where it is heated to 62.5 degree celsius, and then rapidly cooled to 15 degrees and then 4 degrees over the next two hours. After this, it is meticulously labelled and stored in deep freeze storages of -20 C, and tested for bacterial contamination.
“We dispense the milk primarily to premature and extremely sick/vulnerable babies in the NICU, whose mothers are ill themselves, or are experiencing lactation failure,” Khandekar says. “People from outside have also approached us to access PDHM (Pasteurized Donor Human Milk) reserves, but unlike staff, they are unaware of the temperature it is to be stored at, or the window in which it should be consumed. This may end up causing more harm than good.” The reach of milk banks in India, therefore, remains starkly limited–especially when compared to countries like Brazil.
Shortage of PDHM is a persistent reality that milk banks face. “Not every mother admitted in our wards will be willing to donate her milk,” Khandekar says. For every donor who comes forward, there are several newborns in urgent need who go without. The bank operates with a small team, making this work demanding. Counsellors spend their days on their feet, moving endlessly between wards, balancing the urgency of persuasion with the labour of reassuring anxious mothers.
Dr. Fernandez says that milk banks in India face two major barriers: lack of institutional budgets for equipment and staff (most rely on private donations or Rotary support) and the limited number of donors beyond hospital mothers. Khandekar affirms that there is a massive gap in demand and supply. Unlike in other countries where lactation professionals follow up with milk collection at home, and a dense network is set up for supply, India relies mainly on in-hospital donations due to hygiene and storage constraints, severely limiting collections.
Also read: Sivaranjani Santosh's fight to knock mislabelled ORS off the shelf
Scaling up milk banks while promoting breastfeeding, while not a utopian, or fix-it-all solution, could be transformative. This approach eases the burden for mothers coping with delayed lactation, infant health issues, or bereaving the loss of their own child, while ensuring babies get safe nutrition—as opposed to the alternative, which is formula. Dr. Fernandez suggests setting up ‘milk donation camps,’ much like blood donation camps. This however, would require policy changes in budgeting and infrastructural support, and large-scale awareness of breast milk banks, when most of us might have never heard that they exist.
The dominance of formula milk in India is not as much to do with parental choice but the result of systemic neglect. Unless India invests in breastfeeding support and human milk banking, it risks outsourcing infant nutrition to commerce, where formula will continue to fill the gaps—at the cost of its youngest citizens.
Edited by Anushka Mukherjee and Neerja Deodhar
{{quiz}}
Explore other topics
References